by Jena | Apr 9, 2016 | Atrial Fibrillation, Cyclophosphamide, Fludarabine, Graft-versus-host-disease (GvHD), Ileus, Infectious Disease, Melphalan, Sirolimus, Stem Cell Transplant |
Today is Day +7. Dad is doing fairly well considering he is in week two, which is one of the worst weeks that stem cell transplant patients endure. He has experienced a variety of issues as expected.
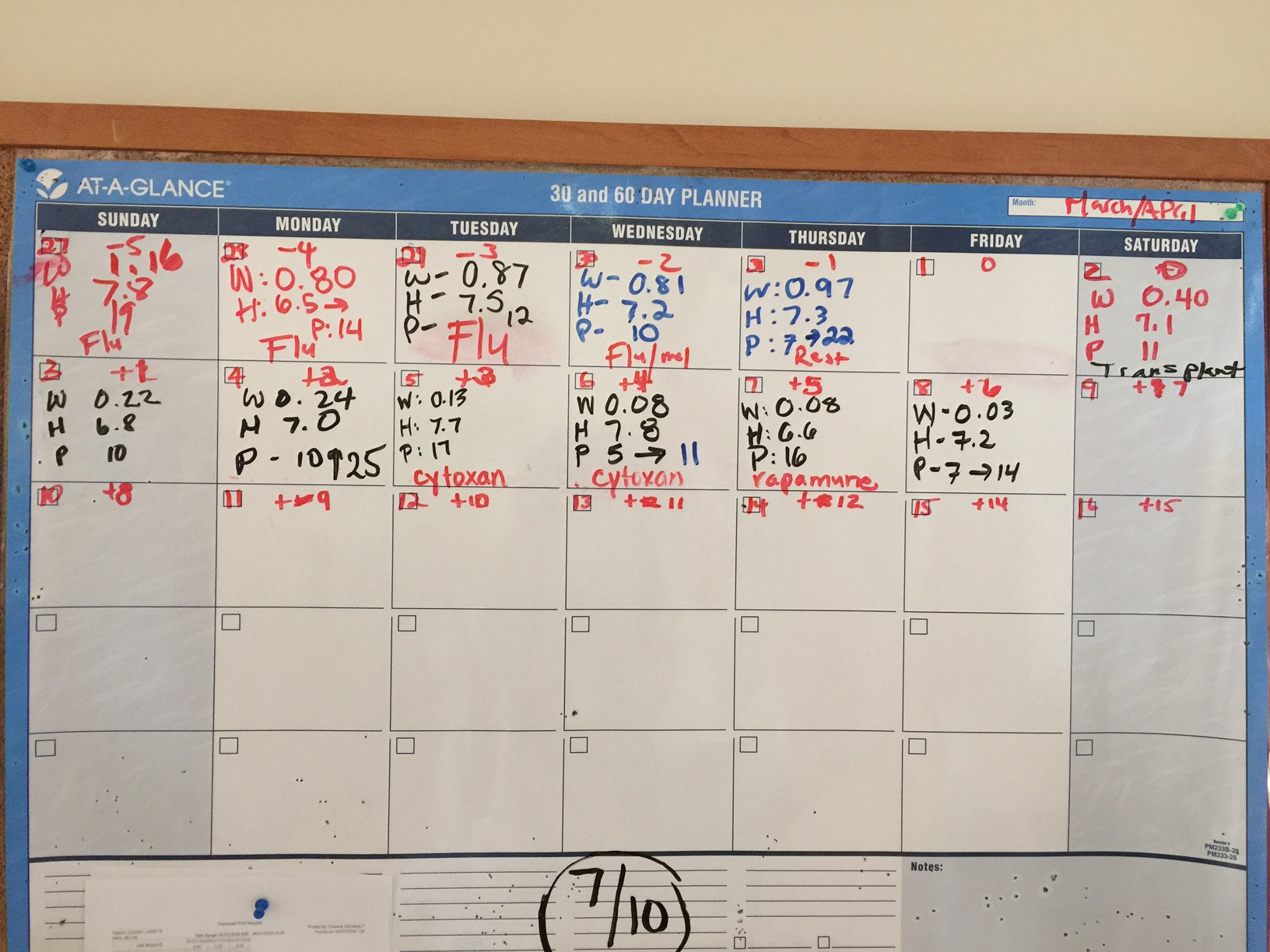
Three blood counts are tracked daily…white blood cell (WBC), hemoglobin (H), and platelets (P). Patients feel the worst as their WBC count plummets to zero, which occurs during week 2.
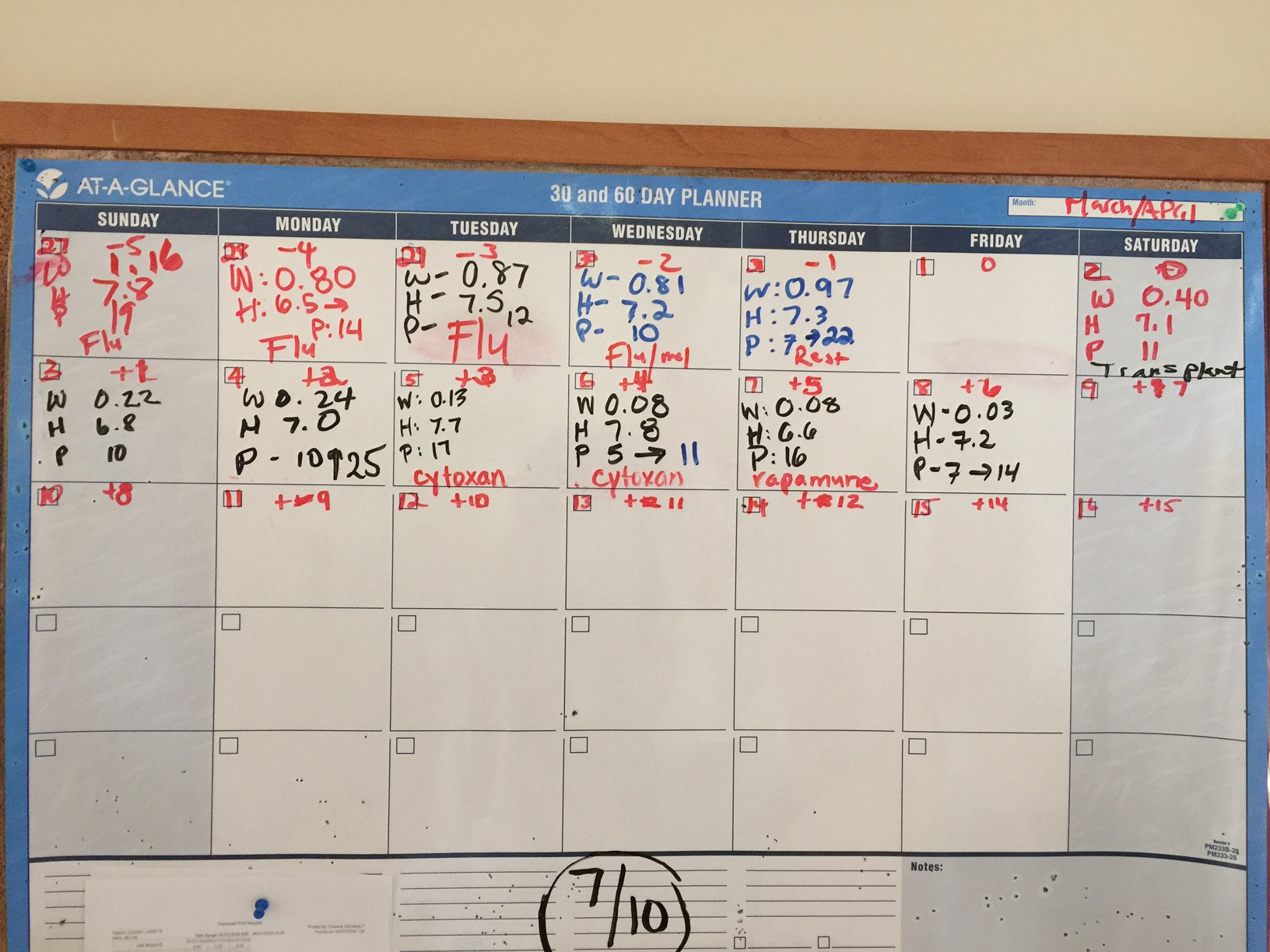
Here’s a recap since I last posted on Day +2.
Day +3, Tuesday, April 5th.
WBC: 0.13 k/uL CRITICAL H: 7.7 g/dL LOW P: 17 k/uL LOW
Dad was fatigued. He complained that he did not sleep well. He was restless. During the day, Dad was napping frequently to catch up on his missed sleep. Dad continued to have diarrhea, which was attributed to the toxicity of the melphalan (one of his two conditioing chemotherapies received on Day -2). Dad was given Imodium to address the diarrhea.
Dad also received his first of two doses of Cytoxin (cyclophosphamide). Post-transplantation cyclophosphamide (Day +3) prevents acute and chronic GvHD (graft-versus-host-disease).
Dad showed no signs of tremors. Doctors believed it was due to toxicity from the fludarabine chemotherapy, which Dad received on Day – 5 through Day – 2.
Day +4, Wednesday, April 6th.
WBC: 0.08 k/uL CRITICAL H: 7.3 g/dL LOW P: 11 k/uL LOW
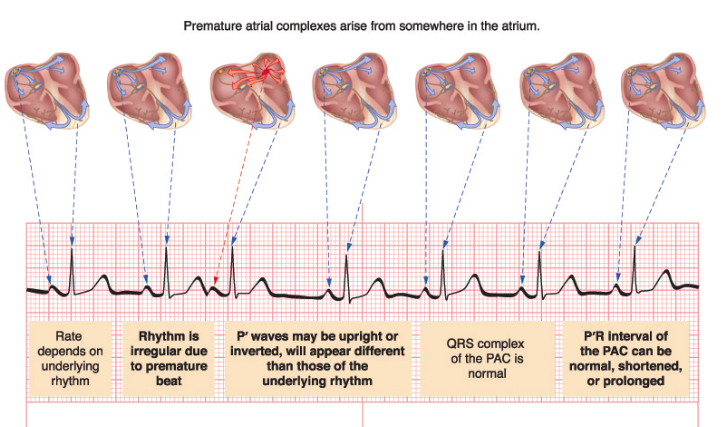
Overnight, Dad had spiked a fever of 101.9 and experienced tachycardia (abnormally rapid heart rate). His heart rate went as high as 175 bpm. He was treated with Lopressor (metoprolol) to help abate the tachycardia. Cardiology was consulted, and two electrocardiograms (ECG) were done (12:43 a.m. and 9:14 a.m.). Both ECGs returned similar results of sinus tachycardia (sinus rhythm with an elevated rated of impulses) with premature atrial complexes (APC).
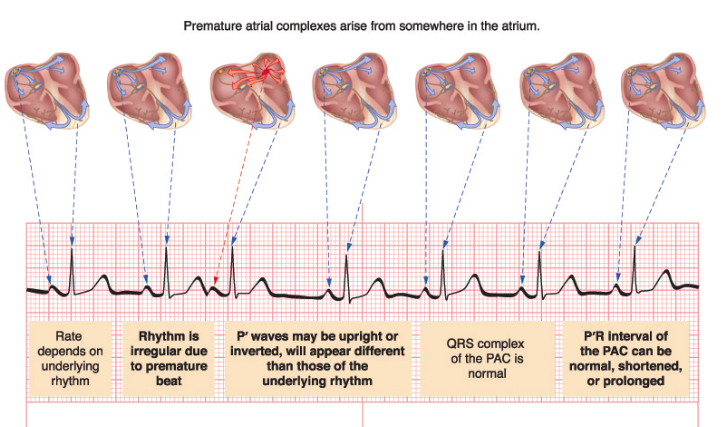
Later mid-afternoon, Dad had an echocardiogram. Dr. Fradley, cardiologist, assessed Dad and concluded that Dad is asymptomatic during these short-lived episodes. He expected that Dad would have arrhythmia due to Dad’s melphalan chemotherapy, which Dad received on Day -2. 12% of patients develop atrial fibrillation from melphalan. He recommended rate control with metoprolol.
Dad had an episode of decreased oxygen saturations. An arterial blood gas (ABG) test was run to measure the acidity (pH) and the levels of oxygen and carbon dioxide in his blood. Dad was put on 3 L/min of oxygen via a nasal cannula.
Dad was also started on Vancomycin via IV to address possible infection in his intestines. Dad continued to have diarrhea and was fatigued. Dad started to note pain in his throat.
Dad was showing signs of fluid retention. He was given two doses of lasix. Dad was having to urinate constantly.
His chest X-ray showed no evidence of pneumonia.
Dad received a platelet transfusion and his second and final dose of Cytoxin (cyclophosphamide).
Day +5, Thursday, April 7th.
WBC: 0.08 k/uL CRITICAL H: 6.6 g/dL LOW P: 16 k/uL LOW
Overnight, Dad went into atrial fibrillation. He was initially given metoprolol via IV. He was then given diltiazem. After Dad experienced low blood pressure and uncontrolled heart rate with diltiazem, he was switched to amiodarone plus digoxin. Dad had another ECG at 8:30 a.m. It was abnormal confirming the atrial fibrillation. Dr. Robinson, cardiology, believed the atrial fibrillation was due to the melphalan chemotherapy, which Dad received on Day -2.
Patients with atrial fibrillation are at greater risk of deep vein thrombosis (DVT). Yet, Dad cannot take an anticoagulant since he is thrombocytopenic (low platetet count).
Dad continued to have diarrhea. He continued to receive Imodium to address. He also continued to receive lasix to address his fluid retention.
Dad complained of tickling of his throat. He was coughing after eating and drinking, thus speech therapy gave him an evaluation. Speech therapy recommended that Dad eat and drink only when sitting up completely. He continued to receive 2 L/min of oxygen.
As planned, Dad was given Rapamune (sirolimus) orally as a prophylaxis against GvHD. He will take sirolimus for 28 days.
Day +6, Friday, April 8th.
WBC: 0.03 k/uL CRITICAL H: 7.2 g/dL LOW P: 14 k/uL LOW
Dad said he received the best night’s sleep he has had in two years. I found that to be quite incredible. The good news was that he was no longer having diarrhea. Dad said his mouth was dry and continued to have discomfort in his throat.
Dad received a platelet transfusion to raise his count from 7 to 14 k/uL.
Late in the morning, Dad finally was up and walking after two to three days of remaining in bed. I brought in a small megaphone for Mom and the physical therapist (PT) to use to encourage Dad to move more. George, the PT, was amused. He had Dad out of bed and moving down the hall with an entourage. Dad was using a walker, and George had a firm grip of the “belt” around Dad’s waist in case Dad fell or collapsed. Dad will have to work himself back up to walking 2 miles a day.


Italian ice is a part of Dad’s new, liquid diet.
Dad had his abdomen X-rayed since it continued to look enlarged. X-ray showed air levels concerning for ileus or obstruction. Patients can develop gastrointestinal (GI) ulcers, vomiting and dairrhea from melphalan. This nasty chemotherapy strips the mucosa of the GI tract. Severe cases can develop ileus or even perforation of the bowel wall. Dad was prescribed Flagyl (metronidazole) as an antibiotic for his abdomen. He was put on a clear liquid diet in order to give his intestines a rest.
Dr. Baluch, BMT (blood & marrow transplant) infectious disease, indicated that Dad would stop receiving vancomycin after today, if he had no more fevers nor positive cultures.
Dad’s urine showed a small amount of blood, but not enough to cause alarm. Another urine analysis to be conducted in one to two days to monitor.
Dad continued to receive lasix to address his fluid retention. He also continued to receive 2 L/min of oxygen.
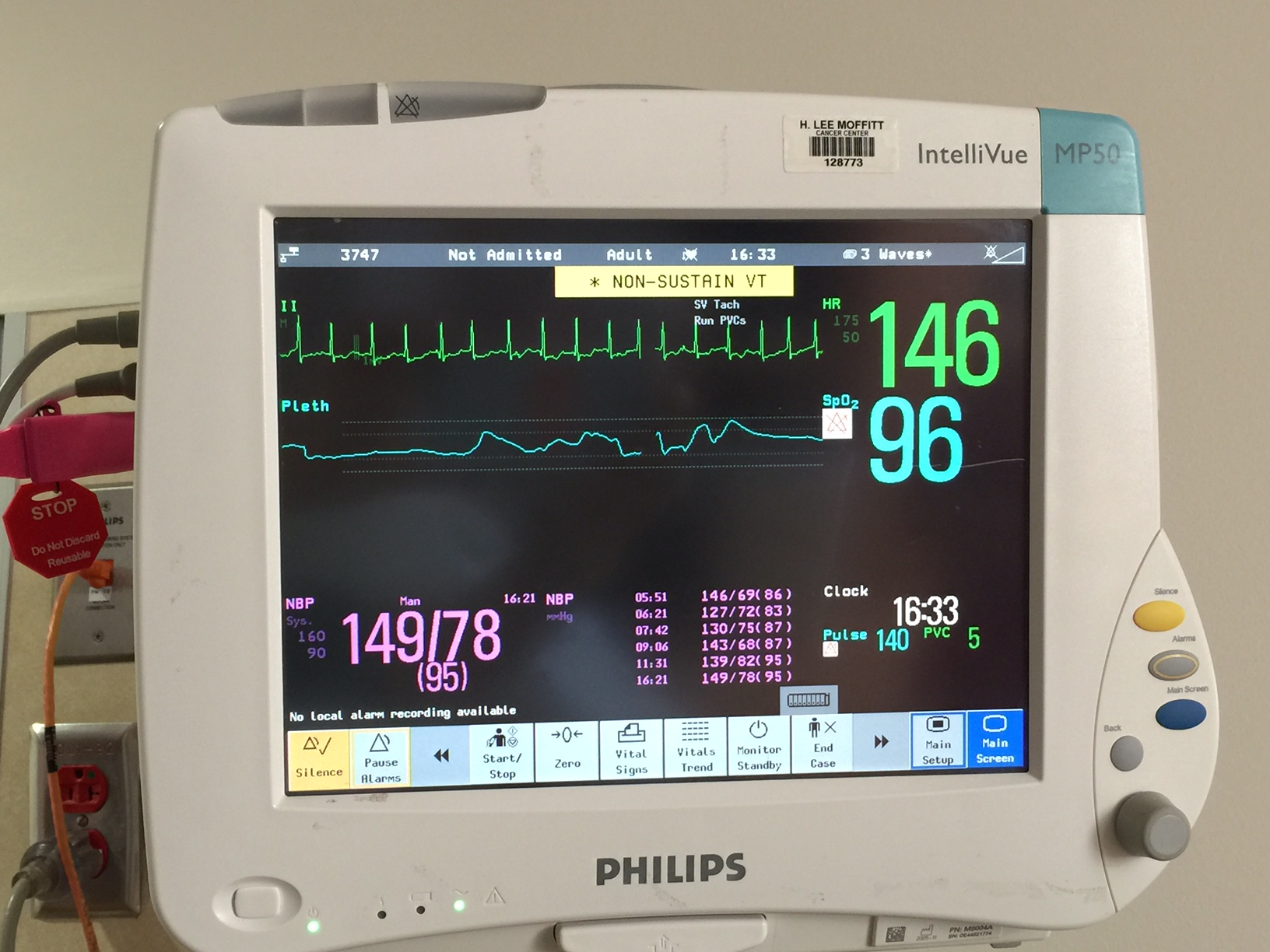
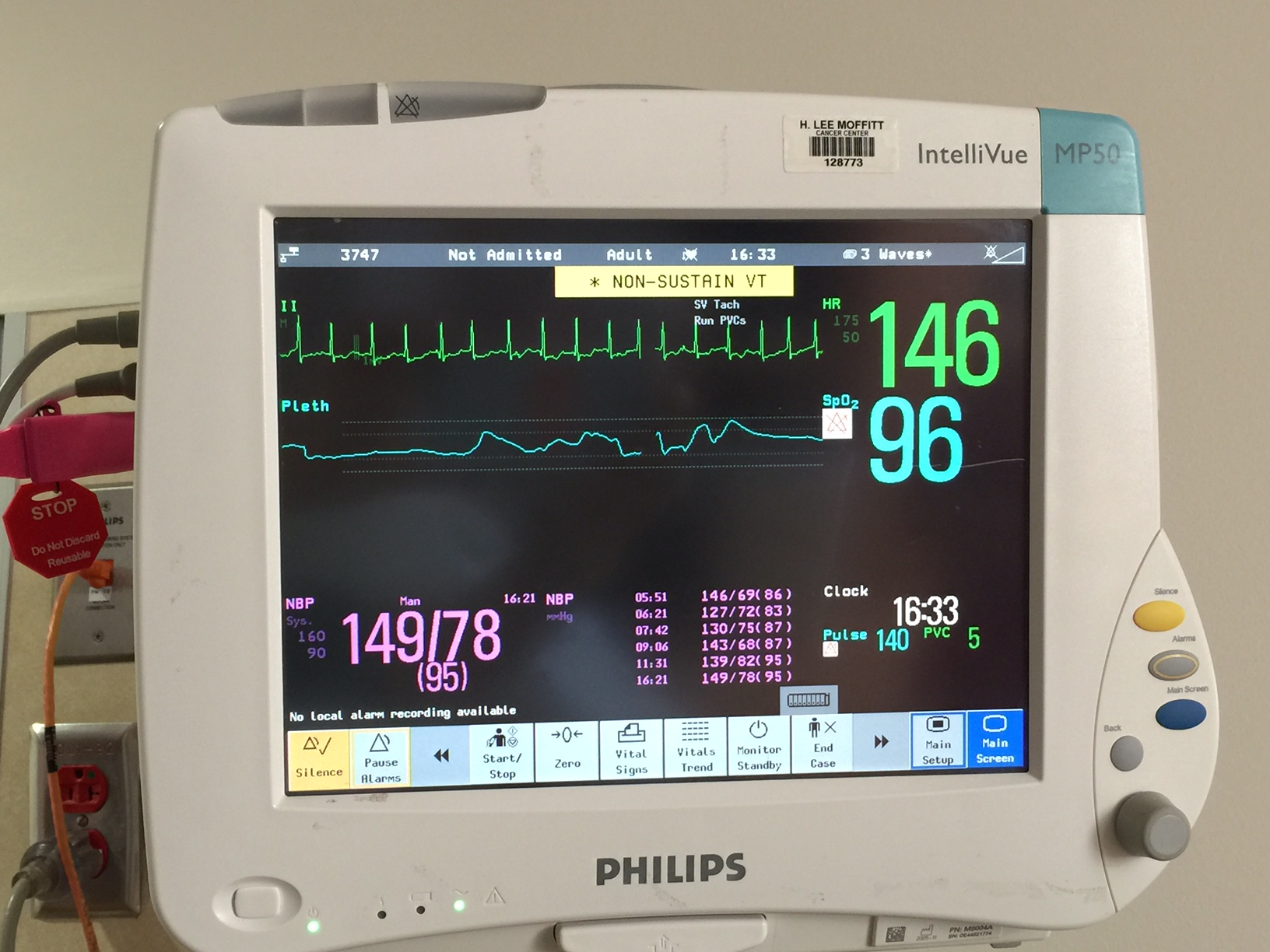
Dad’s heart and oxygen monitor showing 146 bpm.
Late morning, the cardiologist, Dr. Robinson, was thinking that Dad’s heart was improving and had sustained a normal sinus rhythm (NSR). Dr. Robinson had begun to plan how Dad’s heart medications would begin to taper. Unfortunately, Dad’s heart rate was racing again in the afternoon.
by Jena | Apr 1, 2016 | Fludarabine, Melphalan, Stem Cell Transplant |
Today is Dad’s Day 0 while April 1st is more commonly known as April Fool’s Day to the rest of the us.
Husband and I awoke to no AT&T cell phone service. AT&T had a wide spread outage that covered the entire Tampa Bay region and Sarasota. Some AT&T customers thought it was an April Fool’s joke. The outage was caused by cutover issues related to the terribly poor transition of Verizon Fios’ operations to Frontier Communications. The good news was that our household still had internet connectivity (even as a new customer of Frontier Communications) and that Mom and Dad are Verizon cellular customers. We were still able to communicate with Mom and Dad.
Husband picked up Mom at 9:00 a.m. to take her to the Moffitt Cancer Center. Mom and Dad are extremely thankful for Husband chauffeuring Mom back and forth to Moffitt. They are always expressing their gratitude. We are extremely concerned about having Mom ride in one of our cars since Daughter and I are both sick. Dad asked Husband to drive Mom back and forth in a non-contaminated car. Husband has been wiping down the interior of the cars to help reduce the spread of any illness.
After breakfast, Dad learned that his new stems cells had been delayed…until tomorrow, Saturday, April 2nd, in the afternoon. Ugh. Thus, an extra day of rest while Dad pauses Day 0.
Dr. Ochoa, inservice BMT, visited Dad. Dad spoke of two concerns. The first was that the tremors have gotten slightly worse in his hands and arms. Dr. Ochoa believed that it is the chemotherapy affecting Dad’s brain. Dr. Ochoa didn’t believe it is caused by the chemotherapy affecting Dad’s muscles. Dr. Ochoa requested that a neurologist examine Dad. The second issue was that the tops of Dad’s feet are quite red. Dr. Ochoa was not concerned. He believed that the redness may be caused by Dad’s low platelets or the chemotherapy.
When the neurologist came to see Dad, the neurologist was impressed by Dad’s mobility. In fact, when he first saw Dad, he questioned if Dad was even the one he was to examine. This was because the neurologist had spotted Dad walking his two miles. The neurologist came to the same conclusion as Dr. Ochoa…it is chemotherapy affecting Dad’s brain. Based upon the half-lives of the two chemotherapies, fludarabine and melphalan, we anticipate the tremors to stop soon.
Dad’s platelets were fine. His hemoglobin level was a little low so he received one unit of blood.
Both, Daughter and I, went to visit our fabulous family doctor, Dr. Martha Price. I told Dr. Price that Daughter and I need to be healthy again, ASAP. Dr. Price was already familiar with Dad’s situation. She understood the urgent need to be cured with Dad being in the BMT (blood & marrow transplant) unit for his stem cell transplant. I was diagnosed with a sinus infection, and Daughter was diagnosed with bronchitis. Dr. Price went heavy handed, more so than usual because of Dad, with her prescriptions to help speed up our recoveries and to address any possibility of bacterial infection. Dr. Price said that I could not be around Dad for 4 – 5 more days. Daughter was told even longer at 5 – 7 days. That assumes we are feeling good at those points in time.
Midday, I went to Trader Joe’s in an attempt to purchase fruit, salads, sandwiches, and a few frozen meals that Mom can cook in the microwave. Mom has limited options when staying at Moffitt. There is a shared family refrigerator for her to share with others. Mom said it was quite full. There is no proper stove nor oven to cook food…not even a toaster oven…only a microwave. During my grocery shopping, I was texting and snapping and sending photos of a variety of frozen foods that could be cooked in the microwave. Microwaved meals. How unappealing! I tried my best to select dishes that had a hope of tasting palatable. Mom was not interested in most of my offers.



While FaceTiming with Dad yesterday afternoon, Dad was constantly hiccuping. This was believed to be related to the same chemotherapy effects Dad is experiencing with the tremors.
Day 0…the day Dad was to be infused with the donor’s stem cells! April Fool’s!
by Jena | Mar 31, 2016 | Fludarabine, Infectious Disease, Melphalan, Stem Cell Transplant |
Day -5, Sunday, March 27: Dad got settled into his room in the BMT (blood and marrow transplant) unit on the third floor of the Moffitt Cancer Center. His room is just a few doors down from his prior room in early March. Dad met with Dr. Ochoa, inservice BMT doctor, and Karla Adams, inservice BMT physician assistant. Dr. Ochoa is a jokester, which means that Dad will enjoy his visits with Dr. Ochoa. Karla was extremely friendly, as usual, providing Mom and Dad with hugs.
Mid-afternoon, Dad viewed our church’s Easter service online. Afterwards, Dad received some fluids intravenously (saline).
Dad was slightly pleased with his Moffitt dinner and claimed that it was better than before. After Dad finished dinner, he and Mom walked a mile (11 laps in the BMT unit).
Around 9:00 p.m., Dad started receiving pre-meds for his fludarabine (1st of 4), the conditioning chemotherapy. The earlier plan was for Dad to take steroids as a pre-med for each conditioning chemotherapy. However, Dr. Ochoa gave Dad a milder anti-nausea and anti-vomiting pre-med instead. Dad got along fine with these changes. The purpose of the conditioning therapy before a stem cell transplant is to destroy the cancer cells in the body. The dosage received is much higher during conditioning therapy than in the course of normal treatment. Dad didn’t experience any negative side effects during the infusion.
As anticipated, Dad has already met some of his neighbors, Dan and Jamie. Both are younger. Mom and Dad guessed that they are in their 30s. Dan and Jamie are a few days ahead of Dad in the stem cell transplant process.
 Day -4, Monday, March 28: This was Dad’s real birthday. He turned 76!
Day -4, Monday, March 28: This was Dad’s real birthday. He turned 76!
Dad had a good night’s rest. Mom tried out the pull out sofa in Dad’s room last night. She found it to be rather hard. Dad had breakfast and walked one mile in the morning. Dad then saw Dr. Ochoa, who was very pleased with Dad’s status and talking.
Dad saw Dr. Baluch, BMT infectious disease, in the afternoon. She changed one of Dad’s medications and cautioned him as he is very suspectible to infection. His CD4 count was 30. The normal count is 500. Dr. Baluch said that Dad has to be very careful and follow their instructions to minimize the risk of infection.
In the evening, Dad’s pre-meds got started around 9:30 p.m. His fludarabine (2nd of 4) started flowing about 10:00 p.m. He didn’t experience any negative side effects.
Day -3, Tuesday, March 29: Dad had breakfast and then walked a mile. He saw Dr. Ochoa, inservice BMT. Dad’s Moffitt provided lunch was chef salad, pasta with chicken, and carrot cake. Dad spent some time on his laptop. Later in the day, Dad walked two more times at half a mile each. His goal is to walk two miles everyday.
Husband picked Mom up from Moffitt after Dad’s evening shower so that she could do some laundry and get a solid night’s rest at home.
Since we came home from spring break, I haven’t been able to visit Dad, in person, due to my being ill. Each day, Mom and Dad ask if I am feeling better. They are eager to have me visit in person rather than via FaceTime.
Dad received his fludarabine (3rd of 4) later in the evening with no negative effects.
Day -2, Wednesday, March 30: Dad woke up feeling fine. Husband picked up Mom at 9:00 a.m. and took her to the Moffitt Cancer Center. Sweet Daughter had offered to lend Dad her Bose wireless speaker so that Dad could listen to music on his iPhone. Husband visited with Dad and setup the speaker with Dad’s iPhone.
Dr. Ayala, Dad’s BMT doctor, stopped in to visit Dad. This made Mom and Dad very happy.
Mom went to the optional caregivers gathering, which occurs each Wednesday. Mom found it to be interesting and very informative. She learned that each BMT patient, currently in the BMT unit, has a different form of cancer.
This was the last day of Dad’s conditioning  chemotherapies…the double-doozie of fludarabine (4th of 4) and melphalan. Melphalan is the chemotherapy that is likely to give Dad mouth sores, oral mucositis. These usually appear 5 – 10 days after the melphalan is received. Mucositis can then last 7 – 14 days. To minimize Dad’s risk of getting mucositis, Dad used oral cryotherapy. The idea behind the oral cryotherapy is to make the mouth cold enough that the blood vessels in the mouth constrict and reduce the amount of Mephalan in the mouth. Dad packed ice pellets into every nook and cranny of his mouth and contained them in his mouth for 75 minutes. He went through four cupfuls of ice. Dad found it to be quite the challenge. Mom claimed that Dad was screaming while his mouth was full of ice.
chemotherapies…the double-doozie of fludarabine (4th of 4) and melphalan. Melphalan is the chemotherapy that is likely to give Dad mouth sores, oral mucositis. These usually appear 5 – 10 days after the melphalan is received. Mucositis can then last 7 – 14 days. To minimize Dad’s risk of getting mucositis, Dad used oral cryotherapy. The idea behind the oral cryotherapy is to make the mouth cold enough that the blood vessels in the mouth constrict and reduce the amount of Mephalan in the mouth. Dad packed ice pellets into every nook and cranny of his mouth and contained them in his mouth for 75 minutes. He went through four cupfuls of ice. Dad found it to be quite the challenge. Mom claimed that Dad was screaming while his mouth was full of ice.
 Day -1, Thursday, March 31: Dad started his “off day” with a large breakfast of french toast, sausage and donuts. It was an off day in that Dad had a day of rest. No more conditioning chemotherapies. Dad was feeling good and enjoying a new album I gave him for his birthday, Gone Like the Cotton from the Cox Family, which was produced by Alison Krausse. Dad’s favorite song on the album is “Cash on the Barrelhead.”
Day -1, Thursday, March 31: Dad started his “off day” with a large breakfast of french toast, sausage and donuts. It was an off day in that Dad had a day of rest. No more conditioning chemotherapies. Dad was feeling good and enjoying a new album I gave him for his birthday, Gone Like the Cotton from the Cox Family, which was produced by Alison Krausse. Dad’s favorite song on the album is “Cash on the Barrelhead.”
Dad walked his two miles in three phases. Later in the evening, after Dad’s bedtime shower, Husband picked up Mom so that she could get quality sleep in her own bed.
While sitting in his lounger that night, Dad experienced some tremors in both hands and arms.
by Jena | Mar 27, 2016 | Fludarabine, Stem Cell Transplant |
Early in the week, we were notified that Dad’s transplant admission date was moved from Thursday, March 24th to today, Sunday, March 27th per the donor’s request. I have learned that the plan is that it never goes as planned. This delayed admission date, along with Dad’s strong insistence, encouraged me to fly out West on Tuesday to spend spring break with Husband, Son, and Daughter.
How apropos that Dad’s new admission date is Easter Sunday, and our church’s Easter sermon is “New Life Starts Here!”

FaceTiming with Dr. Ayala and Diane
On Thursday while on the mountain, I virtually participated in Dad’s pre-admission appointment with Dr. Ayala, transplant doctor, via FaceTime. I felt comfortable participating virtually since Dad has had two of these appointments in the past prior to his previous admission delays. The appointment was rather routine in that Dad’s medications were reviewed. Dr. Ayala conducted a physical exam. Dr. Ayala confirmed that we were well aware of the risks and acknowledged that we have had this “risk” discussion several times now. Diane, transplant coordinator filling in for Denise, provided an updated calendar depicting day-by-day transplant activities.

Kubi by Revolve Robotics
Dad continues to be amazed by today’s technologies. Husband and I have been discussing additional technologies that would allow us to be in Dad’s room, during his monthlong stay, when we cannot be there the moment the team of doctors make rounds each day. A high-end solution, Double 2 by Double Robotics, is being used in hospitals today. One example is of a teenage lymphoma patient continuing to attend school virtually from his hospital room. I personally like the Kubi by Revolve Robtics as a moderately priced solution.
Dad called the Moffitt Cancer Center this morning to confirm a noon availability of his bed on the BMT (blood & marrow transplant) floor…his bed is ready and waiting for him. If it had not been ready, he would have gone to the BMT clinic at noon to get his first conditioning chemotherapy, Fludarabine, underway while waiting for his bed to become available. During Dad’s Thursday appointment, Diane shared that there are currently 7 or 8 inpatients in progress with their stem cell transplants. Dad will be moving into their BMT neighborhood. Knowing Dad, he will chat them all up within the first few days of admission. I hope they are ready for Chatty Daddy.
Dad’s journey to a new life begins today. Alleluia!
https://youtube.com/watch?v=PBvU7arNhQs%3Frel%3D0






 Day -4, Monday, March 28: This was Dad’s real birthday. He turned 76!
Day -4, Monday, March 28: This was Dad’s real birthday. He turned 76! chemotherapies…the double-doozie of fludarabine (4th of 4) and
chemotherapies…the double-doozie of fludarabine (4th of 4) and  Day -1, Thursday, March 31: Dad started his “off day” with a large breakfast of french toast, sausage and donuts. It was an off day in that Dad had a day of rest. No more conditioning chemotherapies. Dad was feeling good and enjoying a new album I gave him for his birthday,
Day -1, Thursday, March 31: Dad started his “off day” with a large breakfast of french toast, sausage and donuts. It was an off day in that Dad had a day of rest. No more conditioning chemotherapies. Dad was feeling good and enjoying a new album I gave him for his birthday, 

Recent Comments