Day +3 through Day +6
Today is Day +7. Dad is doing fairly well considering he is in week two, which is one of the worst weeks that stem cell transplant patients endure. He has experienced a variety of issues as expected.
Three blood counts are tracked daily…white blood cell (WBC), hemoglobin (H), and platelets (P). Patients feel the worst as their WBC count plummets to zero, which occurs during week 2.
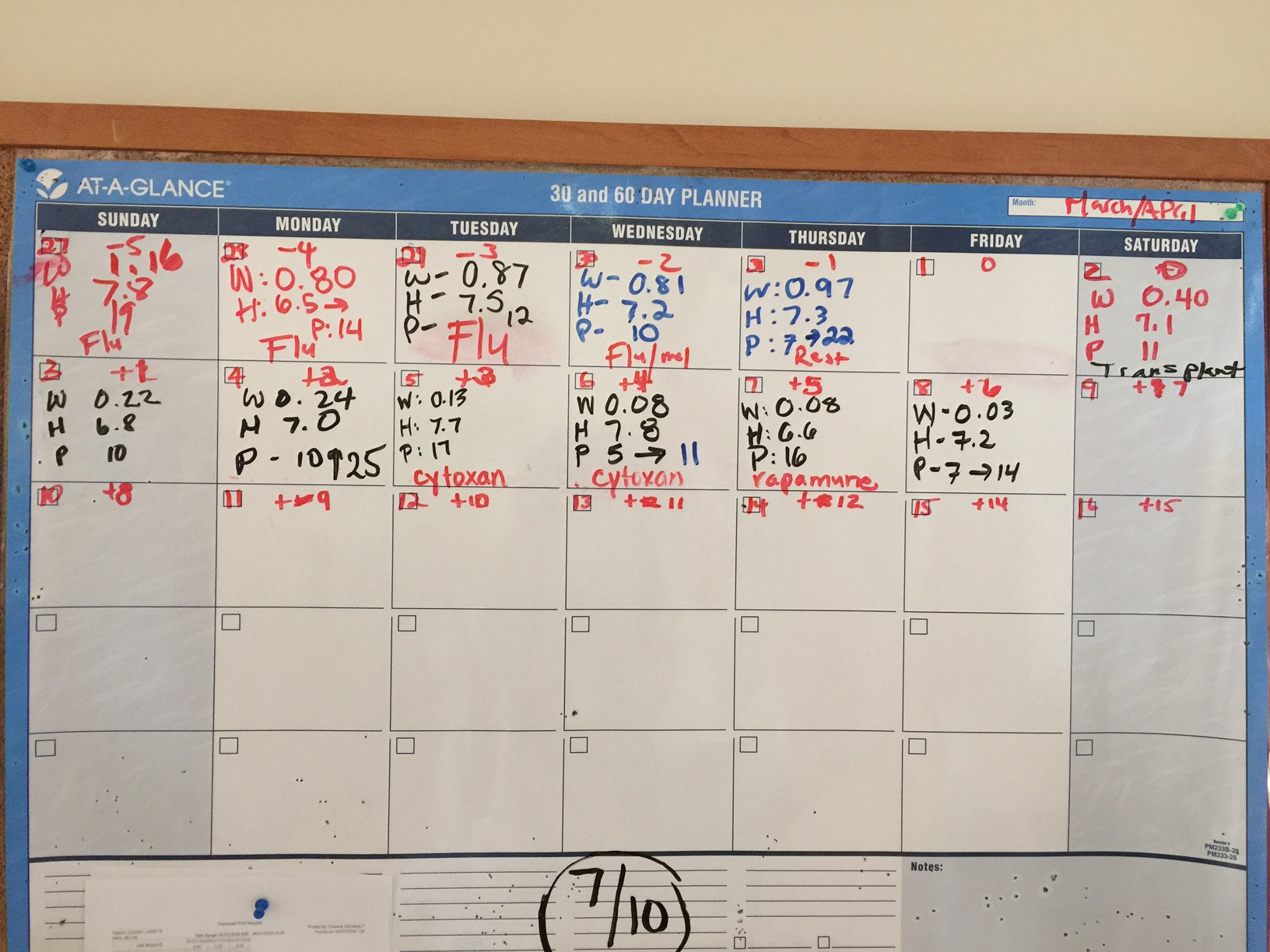
Here’s a recap since I last posted on Day +2.
Day +3, Tuesday, April 5th.
WBC: 0.13 k/uL CRITICAL H: 7.7 g/dL LOW P: 17 k/uL LOW
Dad was fatigued. He complained that he did not sleep well. He was restless. During the day, Dad was napping frequently to catch up on his missed sleep. Dad continued to have diarrhea, which was attributed to the toxicity of the melphalan (one of his two conditioing chemotherapies received on Day -2). Dad was given Imodium to address the diarrhea.
Dad also received his first of two doses of Cytoxin (cyclophosphamide). Post-transplantation cyclophosphamide (Day +3) prevents acute and chronic GvHD (graft-versus-host-disease).
Dad showed no signs of tremors. Doctors believed it was due to toxicity from the fludarabine chemotherapy, which Dad received on Day – 5 through Day – 2.
Day +4, Wednesday, April 6th.
WBC: 0.08 k/uL CRITICAL H: 7.3 g/dL LOW P: 11 k/uL LOW
Overnight, Dad had spiked a fever of 101.9 and experienced tachycardia (abnormally rapid heart rate). His heart rate went as high as 175 bpm. He was treated with Lopressor (metoprolol) to help abate the tachycardia. Cardiology was consulted, and two electrocardiograms (ECG) were done (12:43 a.m. and 9:14 a.m.). Both ECGs returned similar results of sinus tachycardia (sinus rhythm with an elevated rated of impulses) with premature atrial complexes (APC).
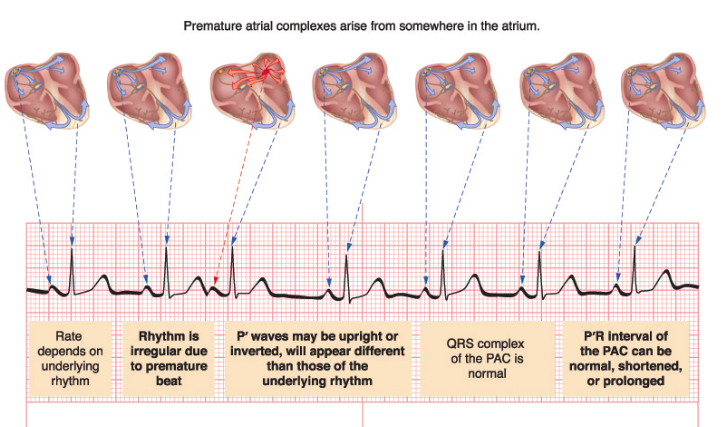
Later mid-afternoon, Dad had an echocardiogram. Dr. Fradley, cardiologist, assessed Dad and concluded that Dad is asymptomatic during these short-lived episodes. He expected that Dad would have arrhythmia due to Dad’s melphalan chemotherapy, which Dad received on Day -2. 12% of patients develop atrial fibrillation from melphalan. He recommended rate control with metoprolol.
Dad had an episode of decreased oxygen saturations. An arterial blood gas (ABG) test was run to measure the acidity (pH) and the levels of oxygen and carbon dioxide in his blood. Dad was put on 3 L/min of oxygen via a nasal cannula.
Dad was also started on Vancomycin via IV to address possible infection in his intestines. Dad continued to have diarrhea and was fatigued. Dad started to note pain in his throat.
Dad was showing signs of fluid retention. He was given two doses of lasix. Dad was having to urinate constantly.
His chest X-ray showed no evidence of pneumonia.
Dad received a platelet transfusion and his second and final dose of Cytoxin (cyclophosphamide).
Day +5, Thursday, April 7th.
WBC: 0.08 k/uL CRITICAL H: 6.6 g/dL LOW P: 16 k/uL LOW
Overnight, Dad went into atrial fibrillation. He was initially given metoprolol via IV. He was then given diltiazem. After Dad experienced low blood pressure and uncontrolled heart rate with diltiazem, he was switched to amiodarone plus digoxin. Dad had another ECG at 8:30 a.m. It was abnormal confirming the atrial fibrillation. Dr. Robinson, cardiology, believed the atrial fibrillation was due to the melphalan chemotherapy, which Dad received on Day -2.
Patients with atrial fibrillation are at greater risk of deep vein thrombosis (DVT). Yet, Dad cannot take an anticoagulant since he is thrombocytopenic (low platetet count).
Dad continued to have diarrhea. He continued to receive Imodium to address. He also continued to receive lasix to address his fluid retention.
Dad complained of tickling of his throat. He was coughing after eating and drinking, thus speech therapy gave him an evaluation. Speech therapy recommended that Dad eat and drink only when sitting up completely. He continued to receive 2 L/min of oxygen.
As planned, Dad was given Rapamune (sirolimus) orally as a prophylaxis against GvHD. He will take sirolimus for 28 days.
Day +6, Friday, April 8th.
WBC: 0.03 k/uL CRITICAL H: 7.2 g/dL LOW P: 14 k/uL LOW
Dad said he received the best night’s sleep he has had in two years. I found that to be quite incredible. The good news was that he was no longer having diarrhea. Dad said his mouth was dry and continued to have discomfort in his throat.
Dad received a platelet transfusion to raise his count from 7 to 14 k/uL.
Late in the morning, Dad finally was up and walking after two to three days of remaining in bed. I brought in a small megaphone for Mom and the physical therapist (PT) to use to encourage Dad to move more. George, the PT, was amused. He had Dad out of bed and moving down the hall with an entourage. Dad was using a walker, and George had a firm grip of the “belt” around Dad’s waist in case Dad fell or collapsed. Dad will have to work himself back up to walking 2 miles a day.


Italian ice is a part of Dad’s new, liquid diet.
Dad had his abdomen X-rayed since it continued to look enlarged. X-ray showed air levels concerning for ileus or obstruction. Patients can develop gastrointestinal (GI) ulcers, vomiting and dairrhea from melphalan. This nasty chemotherapy strips the mucosa of the GI tract. Severe cases can develop ileus or even perforation of the bowel wall. Dad was prescribed Flagyl (metronidazole) as an antibiotic for his abdomen. He was put on a clear liquid diet in order to give his intestines a rest.
Dr. Baluch, BMT (blood & marrow transplant) infectious disease, indicated that Dad would stop receiving vancomycin after today, if he had no more fevers nor positive cultures.
Dad’s urine showed a small amount of blood, but not enough to cause alarm. Another urine analysis to be conducted in one to two days to monitor.
Dad continued to receive lasix to address his fluid retention. He also continued to receive 2 L/min of oxygen.
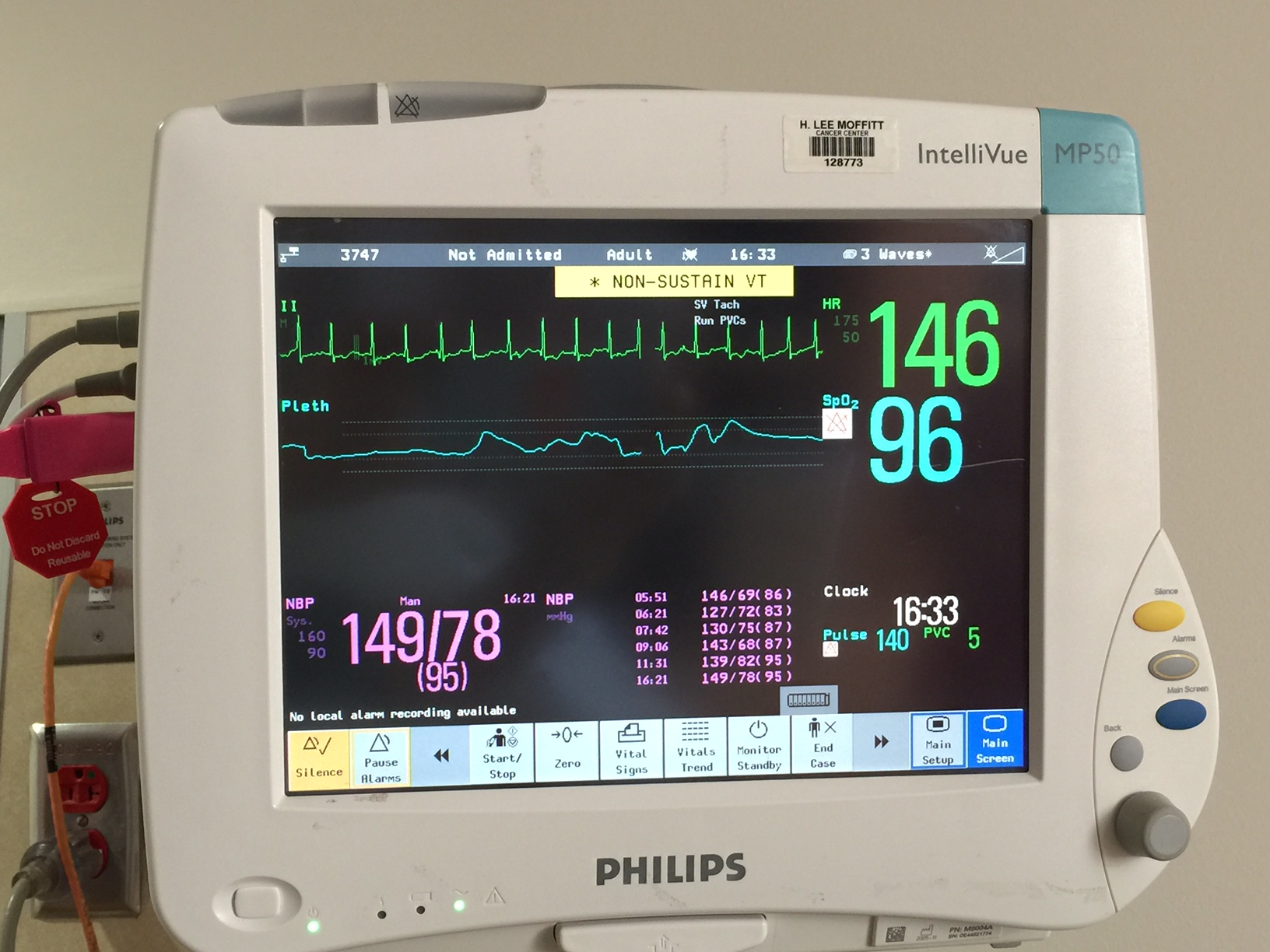
Dad’s heart and oxygen monitor showing 146 bpm.
Late morning, the cardiologist, Dr. Robinson, was thinking that Dad’s heart was improving and had sustained a normal sinus rhythm (NSR). Dr. Robinson had begun to plan how Dad’s heart medications would begin to taper. Unfortunately, Dad’s heart rate was racing again in the afternoon.

Recent Comments