by Jena | Apr 25, 2016 | BK virus, Cytomegalovirus (CMV), Epstein-Barr virus (EBV), Sirolimus, Stem Cell Transplant |
Day +22, Sunday, April 24, 2016
WBC: 2.86 k/uL LOW H: 9.7 g/dL LOW P: 11 k/uL LOW BUN: 83 HIGH Cr: 4.7 CRITICAL Na+: 143 NORMAL
Mentation. Dr. Ochoa-Bayon, inservice BMT, found Dad to be somnolent, but rousable. At times, Dad mumbled and was able to follow some simple commands. Dr. Baluch, BMT infectious disease, found Dad to be less anxious than the day before.
Epstein-Barr Virus, also called the Human Herpesvirus 4, is commonly known as “mono.”
Blood. Dad had a low grade fever during the night. Planned to repeat test for Epstein-Barr Virus (EBV; Human Herpesvirus 4 (HHV-4)) and Cytomegalovirus (CMV; Human Herpesvirus 5 (HHV-5)) on Monday. Set target to keep platelets above 50
A constant challenge is to keep the nurses and technicians, who change every 12 hours, keenly aware of Dad’s thin skin. He has such thin skin as a result of his cancer (CTCL). Nearly all of the medical staff under appreciate how thin Dad’s skin is. They incorrectly assume Mom and I are warning them just because we don’t want a slight tug on his skin. Nearly all types of adhesion (even paper tape) peels Dad’s skin right off. Dad is often left with an open wound when adhesive remover is not used to slowly and methodically to remove medical tape and adhesives. For immunocompromised patients, open wounds pose significant risk for infection.
Dr. Baluch monitored such open wounds on Dad’s chest (adhesive improperly removed during the procedure to remove Dad’s central line catheter last week). She checked on a second open wound on his right, lower back.
No results returned yet from the HHV-6 test conducted the day before.
Lungs. The chest X-Ray, taken the day before, showed an abnormal amount of fluid around Dad’s right lung (pleural effusion) with intermittent collapse or closure of a portion of the lung. Dad continued to be supplemented with oxygen via mask at 3L.
Abdomen. The day before, Dr. Ochoa-Bayona requested an X-ray to confirm the placement of Dad’s feeding tube since Dad had been confused and pulling on his feeding tube. That X-ray prompted the need to further advance the feeding tube. A second X-ray confirmed that it was in the proper place. Dad restarted trickle feeds via his feeding tube. He was monitored for diarrhea. Discontinued D5 water IV and continued free water flushes.
Kidneys. Creatine decreased from 4.9 to 4.7. Dad had good urine output. Dad’s urine remained slightly bloody due to the BK virus. This prompted Dr. Ochoa-Bayona, inservice BMT, to reduce the amount of sirolimus (immunosuppressant) Dad received.
by Jena | Apr 25, 2016 | Dialysis, Epstein-Barr virus (EBV), HHV-6, Stem Cell Transplant |
Day +21, Saturday, April 23, 2016
WBC: 2.67 k/uL LOW H: 7.6 g/dL LOW P: 21 k/uL LOW BUN: 85 HIGH Cr: 4.9 CRITICAL Na+: 145
Mentation. Dad was sleepy and lethargic when Dr. Ochoa-Bayona, inservice BMT, visited. Yet, Dr. Ochoa-Bayon was able to arouse him. Dad had insensible speech. Dr. Baluch switched Dad from voriconazole, his antifungal therapy, to micafungin due to concern of voriconazole playing a role in Dad’s altered mentation.
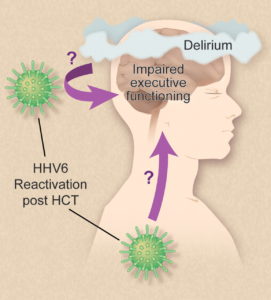
An HHV-6 test was ordered.
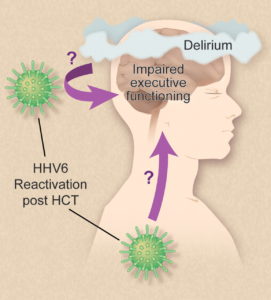
Illustration by Debra Dartez.
According to the HHV-6 Foundation, Human Herpesvirus 6 (HHV-6) is comprised of two closely related herpes viruses (HHV-6A and HHV-6B) that infect nearly all humans before the age of two. It has a life-long latency and can become reactivated later in life. In some cases, HHV-6 reactivation in the brain tissue can cause cognitive dysfunction, permanent disability and death.
Considered a lumbar puncture (LP; aka spinal tap), which would require Dad’s platelets to be 50 k/uL. LP would test for Epstein-Barr Virus (EBV) in Dad’s central nervous system (CNS).
Blood. Dad had a low grade fever the day before. His PICC line was tested with no negative results. Dad’s arterial blood gas (ABG) showed respiratory Alkalosis (pH 7.49), which is an excessively alkaline condition of the body fluids or tissues.
Lungs. Dad was supplemented with oxygen via mask at 4L. He continued to have strong coughs.
Abdomen. Diarrhea improved. Dr. Ochoa-Bayona wanted an X-ray to confirm the placement of Dad’s feeding tube since Dad had been confused and pulling on his feeding tube. Dad’s feeding was restarted (trickle feed) via feeding tube after X-ray taken.
Kidneys. Urine output improved again. His urine was slightly bloody again since his urinary catheter (aka foley) was replaced. No dialysis was needed since Dad’s creatine/electrolytes were stable.
by Jena | Apr 24, 2016 | Atrial Fibrillation, Cytomegalovirus (CMV), Dialysis, Epstein-Barr virus (EBV), Graft-versus-host-disease (GvHD), Ileus, Meropenem, Minocycline, Sirolimus, Stem Cell Transplant |
Day +14, Saturday, April 16th.
WBC: 0.06 k/uL CRITICAL H: 7.7 g/dL LOW P: 10 k/uL LOW Cr: 5.1 CRITICAL Na+: 152 CRITICAL
Blood. The atypical Gram-negative bacteria was finally identified as Achromobacter xylosoxidans. Looks like an extremely difficult spelling bee word. He Continued minocycline for MRSA.
Dad continued to receive blood support (platelet and blood transfusions & neupogen shots) as needed.
Graft versus host disease (GvHD). Dad was still unable to take sirolimus since he was restricted from all food and drink.
Mouth & Throat. Dad continued to have pain from mucositis and used magic mouthwash to treat.
Heart. Overnight, Dad had an episode of tachycardia, which is an abnormal heart rate. He received metoprolol to address. His heart rate improved, however his blood pressure dropped. Cardiology came by later.
Lungs. Mom was very stressed about Dad being fed and that he did not have a feeding tube. Later in the evening, they were able to finally successfully place Dad’s feeding tube. Continued voriconazole and acycolovir.
Doctor sought to wean Dad off supplemental oxygen.
Abdomen. Dad continued meropenem, an ultra-broad spectrum antibiotic.
Kidneys. Dad was put on dialysis last night. First, he had a central venous catheter, which is a catheter used for dialysis, placed in his right groin. The surgeon wanted to place the dialysis catheter in his upper right chest above his heart, but Dad’s central line catheter is already occupying that spot. The surgeon did not want to place it in Dad’s upper left chest since the tubing would require a curve to get to Dad’s heart. The groin was not an optimal location either for two reasons. A groin placement would make it painful for Dad to sit, and Dad would be at a greater risk for a blood clot. The surgeon suggested that in 4 – 5 days, Dad should have his central line catheter moved away from his upper right chest and have the dialysis catheter moved from his right groin to his upper right chest. It was clear that the surgeon did not want the dialysis catheter to remain in Dad’s groin for too long.
Before Dad could have his dialysis catheter placed, he needed to get his platelet count to 50. Dad required three bags of platelets. Without enough platelets, Dad would have had trouble clotting during the catheter insertion procedure. He also received a bag of plasma and a bag of blood. Thank you to all those who regularly donate these blood products. Dad is a large consumer!
Day +15, Sunday, April 17th.
WBC: 0.13 k/uL CRITICAL H: 8.7 g/dL LOW P: 79 k/uL LOW Cr: 3.4 HIGH Na+: 147 HIGH
Blood. Dad’s white blood cell count continued to rise. His central line catheter continued to test positive for the atypical Gram-negative bacteria, Achromobacter xylosoxidans. Continued minocycline.
Dad continued to receive blood support (platelet and blood transfusions & neupogen shots) as needed.
Graft versus host disease (GvHD). Sirolimus was restarted since the feeding tube was inserted.
Mouth & Throat. Dad continued to have pain from mucositis and used magic mouthwash to treat.
Heart. Dad blood pressure improved and remained stable.
Lungs. Dad continued to receive supplemental oxygen. Continued voriconazole and acycolovir.
Abdomen. Dad continued meropenem, an ultra-broad spectrum antibiotic. The prior day’s CT scan showed evidence of ileus, which is the inability of the intestine to contract normally and move waste out of Dad’s body.
Kidneys. Dad no longer had blood in his urine. He remained on continuous dialysis. The prior day’s CT scan also showed hydronephrosis, excess fluid in the kidney due to a backup of urine, and hydroureter, dilated ureter. Urology was consulted.
Day +16, Monday, April 18th.
WBC: 0.24 k/uL CRITICAL H: 8.9 g/dL LOW P: 41 k/uL LOW Cr: 1.9 HIGH Na+: 143 NORMAL

Doughnuts from the Mini Doughnut Factory for the ICU staff.
Blood. Dad’s white blood cell count continued to rise. Dad continued to receive blood support (platelet and blood transfusions & neupogen shots) as needed. Weekly testing of CMV and EBV showed positive with decreasing levels. Thus, no treatment prescribed, but will continue to monitor. Dad continued to receive minocycline.
Graft versus host disease (GvHD). Dad continued to receive sirolimus via feeding tube. Acute GvHD assessment resulted in an overall grade of 0.
- Skin = Stage 0
- Liver = Stage 0
- Gut = Stage 0
Mouth & Throat. Dad continued to have pain from mucositis, grade 1, and used magic mouthwash to treat.
Heart. Dad was in and out of atrial fibrillation. Continued metoprolol to address. Blood pressure continued its improvement.
Lungs. Continued voriconazole and acycolovir. Dad continued to receive supplemental oxygen, but lowered oxygen flow from 10L to 6L. Continued to have productive coughs. Kept Dad more upright in bed (no less than 30 degrees).
Abdomen. Began tube feeds to provide Dad nutrition. X-ray taken.
Kidneys. Dad remained on continuous dialysis. Doctor considered moving Dad from continuous dialysis to 4 hour dialysis.
Day +17, Tuesday, April 19th.
WBC: 0.55 k/uL CRITICAL H: 9.2 g/dL LOW P: 40 k/uL LOW Cr: 2.3 HIGH Na+: 145 NORMAL
Blood. Dad had his central line catheter removed. It was an extremely painful event. The surgical scissors/tweezer tip broke off and remained in Dad’s chest near his right, third rib. The broken piece was subsequently retrieved. Later another painful event for Dad was that the PICC team was unsuccessful in placing a PICC line in Dad’s arm.
He continued to receive minocycline.
Dad’s white blood cell count continued to rise. Dad continued to receive blood support (platelet and blood transfusions & neupogen shots) as needed.
Graft versus host disease (GvHD). Dad continued to receive sirolimus via feeding tube. Acute GvHD assessment resulted in an overall grade of 0.
- Skin = Stage 0
- Liver = Stage 0
- Gut = Stage 0
Mouth & Throat. Dad continued to have pain from mucositis, grade 1, and used magic mouthwash to treat.
Heart. Dad was in and out of atrial fibrillation. Continued metoprolol to address. Cardiology was following.
Lungs. Dad continued to receive supplemental oxygen, but lowered oxygen flow from 6L to 2L. Continued to have productive coughs. Continued voriconazole and acycolovir.
Abdomen. Continued tube feeds.
Kidneys. Dad had no dialysis. Considered moving Dad back to BMT (Blood & Marrow Transplant) unit from ICU.
Mentation: Dad was disoriented to place and time.
by Jena | Apr 17, 2016 | Atrial Fibrillation, BK virus, Epstein-Barr virus (EBV), Folotyn, Ileus, Infectious Disease, Lasix, MRSA, Rituximab, Stem Cell Transplant, Vancomycin, Zosyn |
Catching you up from last Saturday to Wednesday…
Day +7, Saturday, April 9th.
WBC: 0.03 k/uL CRITICAL H: 7.3 g/dL LOW P: 16 k/uL LOW
Dad had continued to go in and out of atrial fibrillation. By the evening, his heart was in normal sinus rhythm (NSR). Dad felt that his abdomen had improved.
Dad noticed increasing throat pain with swallowing. Oral mucositis (mouth sores) can be extremely painful and can result in an inability to eat, speak, or swallow. Last summer, when Dad had received Folotyn (pralatrexate) chemotherapy, he had suffered from oral mucositis. Dad had used magic mouthwash to get some relief. Magic mouthwash is the term given to a solution used to treat oral mucositis.
Abdominal fluid retention improved slightly. Dad had an abdominal X-ray taken.
His diarrhea remained improved. He remained fever free. He remained on 2 L/min oxygen.
MRSA was confirmed on April 6th once Staphylococcus was identified on April 5th.
Day +8, Sunday, April 10th.
WBC: 0.01 k/uL CRITICAL H: 7.3 g/dL LOW P: 13 k/uL LOW
Report from the day before’s abdominal X-ray showed mildly prominent loops in his small intestine, which possibly represented ileus or enteritis. Ileus is the inability of the intestine to contract normally and move waste out of the body. Enteritis is inflammation of the intestine usually accompanied with diarrhea. Dad’s diet was downgraded to clear liquids. His abdominal swelling was improved, yet he continued to receive lasix, a diuretic, to address the fluid retention.
Dad had an X-ray of his chest taken. He was breathing on his own.
Dad switched to an oral amiodarone to manage his atrial fibrillation.
He continued to be monitored for EBV (Epstein-Barr virus), which is more commonly known as mononucleosis or “mono.” Most people will be infected with EBV in their lifetime and will not have any symptoms since it is controlled by a healthy immune system. Yet, when someone has a weakened immune system, the EBV infection can get out of control.
Day +9, Monday, April 11th.
WBC: 0.04 k/uL CRITICAL H: 8.2 g/dL LOW P: 5 k/uL CRIT
The prior day’s chest X-ray suggested inflammation in Dad’s lungs versus fluid overload. Dad’s respiratory culture showed both “gram-positive” and “gram-negative.” These are terms used to classify bacteria into two groups. Usually, gram-positive bacteria are helpful, and gram-negative are the ones that cause illness.
Dad’s atrial fibrillation continued to be addressed with the oral amiodarone. He continued to receive lasix, a diuretic, to address the fluid retention. Dad remained on a clear liquid diet.
The blood in Dad’s urine was suspected to be the BK virus and adenovirus. For most, the BK virus has no consequences since it remains latent, but it can be reactivated during post stem cell transplant when immunosuppressed.
Dad was too tired to work with physical therapy.
Day +10, Tuesday, April 12th.
WBC: 0.02 k/uL CRITICAL H: 8.2 g/dL LOW P: 7 k/uL CRIT
Dad started to choke/cough when eating ice or drinking liquids. Yet, Dad said that his cough had improved and was no longer producing sputum, which is a mixture of saliva and mucus. Respiratory culture from the day before likely indicated MRSA.
Dad’s sodium was high at 148 mmol/L..
Day +11, Wednesday, April 13th.
WBC: 0.01 k/uL CRITICAL H: 8.0 g/dL LOW P: 12 k/uL LOW
Dad continued to be monitored for EBV. Based upon the latest EBV test results, Dr. Ayala, Dad’s primary BMT doctor, was consulted. It was determined that Dad would receive an infusion of rituximab. Rituximab is used to treat EBV post stem cell transplant. Since Dad experienced rigors, fatigue and mild confusion in the morning, the rituximab treatment was postponed.
Dad complained of further pain in his mouth and throat. Dad continued to take oxycodone and magic mouthwash to provide relief from the mucositis. Two X-rays were taken (chest and abdomen). Dad restarted supplemental oxygen.
His cultures indicated MRSA. Dad was started on two new antibiotics, vancomycin and Zosyn (piperacillin/tazobactam). Vancomycin is used to treat infection of the intestines. Zosyn is the combination of two penicillins.
Dad experienced an abnormal heart rate last night, which was resolved with metoprolol. Dad’s atrial fibrillation continued to be addressed with the oral amiodarone. He continued to receive lasix, a diuretic, to address the fluid retention. Dad remained on a clear liquid diet. Dad had a foley catheter placed since he was at a high fall risk. Dad was given Imodium to treat his diarrhea.
Adenovirus was ruled out as the cause of blood in Dad’s urine. BK virus was still a possibility. Set a goal to maintain Dad’s platelets at 20.
Dad’s sodium was high again at 147 mmol/L. Dr. Baluch, BMT infectious disease, noted that Dad’s T. bilirubin was mildly elevated and wanted to monitor trend.


Recent Comments