by Jena | Apr 25, 2016 | Dialysis, Epstein-Barr virus (EBV), HHV-6, Stem Cell Transplant |
Day +21, Saturday, April 23, 2016
WBC: 2.67 k/uL LOW H: 7.6 g/dL LOW P: 21 k/uL LOW BUN: 85 HIGH Cr: 4.9 CRITICAL Na+: 145
Mentation. Dad was sleepy and lethargic when Dr. Ochoa-Bayona, inservice BMT, visited. Yet, Dr. Ochoa-Bayon was able to arouse him. Dad had insensible speech. Dr. Baluch switched Dad from voriconazole, his antifungal therapy, to micafungin due to concern of voriconazole playing a role in Dad’s altered mentation.
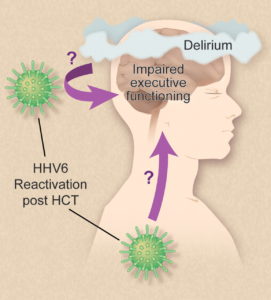
An HHV-6 test was ordered.
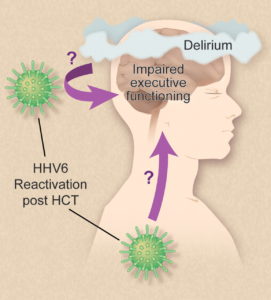
Illustration by Debra Dartez.
According to the HHV-6 Foundation, Human Herpesvirus 6 (HHV-6) is comprised of two closely related herpes viruses (HHV-6A and HHV-6B) that infect nearly all humans before the age of two. It has a life-long latency and can become reactivated later in life. In some cases, HHV-6 reactivation in the brain tissue can cause cognitive dysfunction, permanent disability and death.
Considered a lumbar puncture (LP; aka spinal tap), which would require Dad’s platelets to be 50 k/uL. LP would test for Epstein-Barr Virus (EBV) in Dad’s central nervous system (CNS).
Blood. Dad had a low grade fever the day before. His PICC line was tested with no negative results. Dad’s arterial blood gas (ABG) showed respiratory Alkalosis (pH 7.49), which is an excessively alkaline condition of the body fluids or tissues.
Lungs. Dad was supplemented with oxygen via mask at 4L. He continued to have strong coughs.
Abdomen. Diarrhea improved. Dr. Ochoa-Bayona wanted an X-ray to confirm the placement of Dad’s feeding tube since Dad had been confused and pulling on his feeding tube. Dad’s feeding was restarted (trickle feed) via feeding tube after X-ray taken.
Kidneys. Urine output improved again. His urine was slightly bloody again since his urinary catheter (aka foley) was replaced. No dialysis was needed since Dad’s creatine/electrolytes were stable.
by Jena | Apr 24, 2016 | BK virus, Dialysis, Infectious Disease, Stem Cell Transplant |
Day +19, Thursday, April 21, 2016
WBC: 1.43 k/uL LOW H: 8.5 g/dL LOW P: 18 k/uL LOW BUN: 83 HIGH Cr: 4.3 CRITICAL Na+: 150 HIGH
Mentation. Dad was alert when Dr. Ochoa-Bayona, inservice BMT, visited. He oriented to person, place, and time, but he closed his eyes during conversations. Dad was mildly confused when Dr. Baluch, BMT infectious disease, visited.
Blood. Repeated testing for BK virus. Got D5 water IV.
Mouth and Throat. Dad requested ice chips, but was still not permitted due to aspiration risk.
Lungs. Dad continued to breathe on his own. He continued to cough and have thick secretions from the mucositis.
Abdomen. Diarrhea continued. Dad’s feeding was still suspended due to the diarrhea.
Kidneys. Urine output improved again. Saw a slight increase in creatine (Cr). Monitored sodium (Na+). Urine culture conducted.
Day +20, Friday, April 22, 2016
WBC: 2.34 k/uL LOW H: 8.2 g/dL LOW P: 14 k/uL LOW BUN: 85 HIGH Cr: 4.8 CRITICAL Na+: 148 HIGH
Mentation. When Dr. Ochoa-Bayona, inservice BMT, visited in the morning, he found Dad to be more confused than the previous day. Dad could only orient to a person. Dad didn’t know where he was nor the date. He was slurring his speech. Dad remained in a confused state when Dr. Chemaly, nephrology, visited midday. Dad would only repeat back what Dr. Chemaly said. When Dr. Baluch, BMT infectious disease, came by in the evening, she felt that Dad had worsened confusion.
An EEG was performed, which tested Dad’s cerebral function. The result was abnormal and initially suggested nonspecific moderate to severe brain malfunction. No seizure activity was observed during the study. Dad’s case was reevaluated and noted that Dad had experienced acute renal (kidney) failure, BUN level was high at 85, and creatine (Cr) was trending down.
A CT scan of Dad’s brain indicated no acute cerebral lesions but did show that Dad’s sinuses were irritated and inflamed.
An MRI of Dad’s brain showed no acute changes. The MRI ruled out stroke and abscess.
Dad’s mental state to be pursued as caused by infection, toxins or metabolic problems. Dr. Chemaly believed that Dad’s mental state was unlikely due to uremia, a condition involving abnormally high levels of waste products in Dad’s blood.
Dr. Ochoa-Bayona withheld narcotics and sedatives.
Blood. Increased D5 water IV.
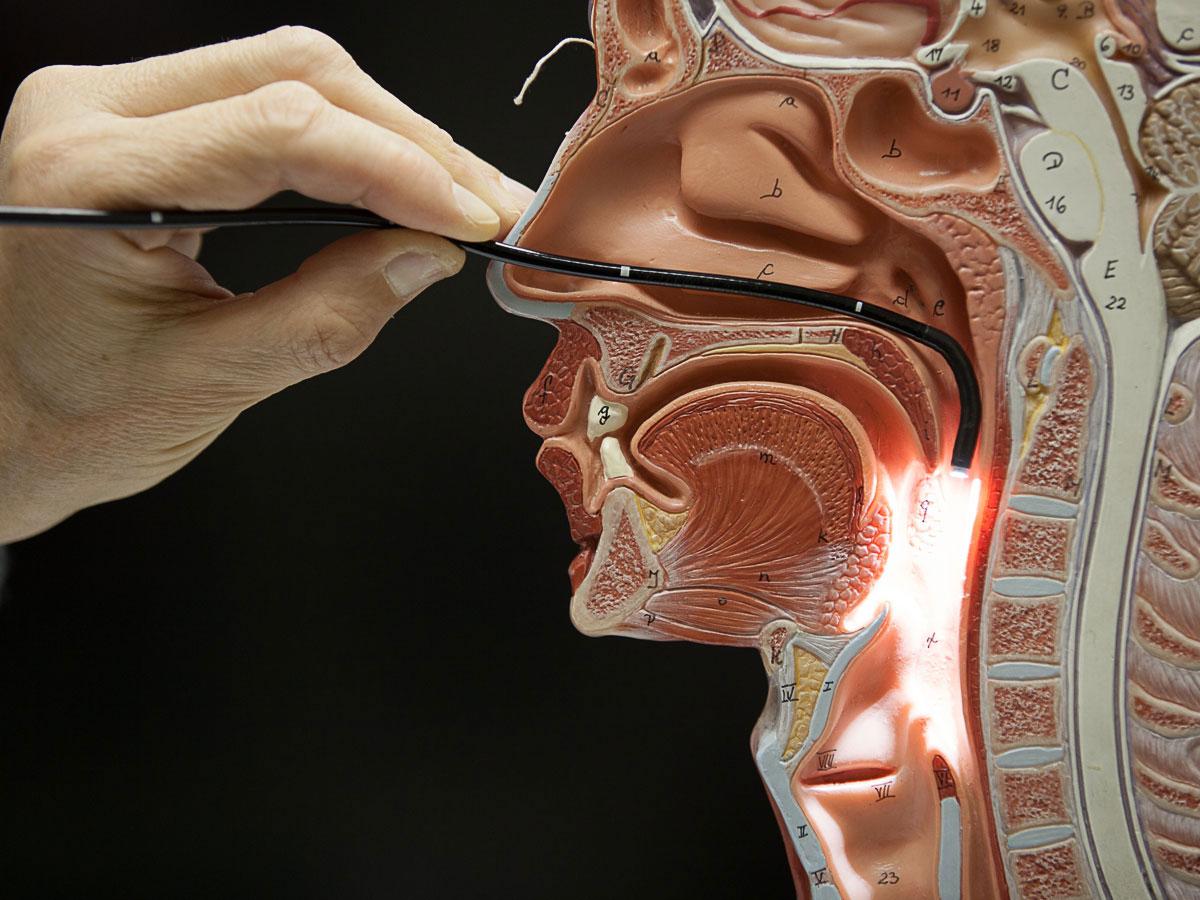 Mouth and Throat. Based upon the result of the CT scan of Dad’s brain, ENT (ear, nose & throat) was consulted to check for fungal sinusitis. ENT performed a bedside Flexible Nasal Endoscopy, which showed no evidence of a fungal infection. It did show a clear, runny nose. ENT recommended continued IV antibiotics for viral and bacterial sinusitis.
Mouth and Throat. Based upon the result of the CT scan of Dad’s brain, ENT (ear, nose & throat) was consulted to check for fungal sinusitis. ENT performed a bedside Flexible Nasal Endoscopy, which showed no evidence of a fungal infection. It did show a clear, runny nose. ENT recommended continued IV antibiotics for viral and bacterial sinusitis.
Lungs. Dad was placed back on supplemental oxygen at 2L. He continued to cough and have thick secretions from the mucositis.
Abdomen. Dad’s feeding was still suspended.
Kidney. Dad’s urine output continued to improve and no longer contained blood. Dr. Chemaly, nephrology, wanted to avoid dialysis given the possibility of an ischemic stroke, which occurs as a result of an obstruction within a blood vessel supplying blood to the brain.
by Jena | Apr 24, 2016 | Atrial Fibrillation, Cytomegalovirus (CMV), Dialysis, Epstein-Barr virus (EBV), Graft-versus-host-disease (GvHD), Ileus, Meropenem, Minocycline, Sirolimus, Stem Cell Transplant |
Day +14, Saturday, April 16th.
WBC: 0.06 k/uL CRITICAL H: 7.7 g/dL LOW P: 10 k/uL LOW Cr: 5.1 CRITICAL Na+: 152 CRITICAL
Blood. The atypical Gram-negative bacteria was finally identified as Achromobacter xylosoxidans. Looks like an extremely difficult spelling bee word. He Continued minocycline for MRSA.
Dad continued to receive blood support (platelet and blood transfusions & neupogen shots) as needed.
Graft versus host disease (GvHD). Dad was still unable to take sirolimus since he was restricted from all food and drink.
Mouth & Throat. Dad continued to have pain from mucositis and used magic mouthwash to treat.
Heart. Overnight, Dad had an episode of tachycardia, which is an abnormal heart rate. He received metoprolol to address. His heart rate improved, however his blood pressure dropped. Cardiology came by later.
Lungs. Mom was very stressed about Dad being fed and that he did not have a feeding tube. Later in the evening, they were able to finally successfully place Dad’s feeding tube. Continued voriconazole and acycolovir.
Doctor sought to wean Dad off supplemental oxygen.
Abdomen. Dad continued meropenem, an ultra-broad spectrum antibiotic.
Kidneys. Dad was put on dialysis last night. First, he had a central venous catheter, which is a catheter used for dialysis, placed in his right groin. The surgeon wanted to place the dialysis catheter in his upper right chest above his heart, but Dad’s central line catheter is already occupying that spot. The surgeon did not want to place it in Dad’s upper left chest since the tubing would require a curve to get to Dad’s heart. The groin was not an optimal location either for two reasons. A groin placement would make it painful for Dad to sit, and Dad would be at a greater risk for a blood clot. The surgeon suggested that in 4 – 5 days, Dad should have his central line catheter moved away from his upper right chest and have the dialysis catheter moved from his right groin to his upper right chest. It was clear that the surgeon did not want the dialysis catheter to remain in Dad’s groin for too long.
Before Dad could have his dialysis catheter placed, he needed to get his platelet count to 50. Dad required three bags of platelets. Without enough platelets, Dad would have had trouble clotting during the catheter insertion procedure. He also received a bag of plasma and a bag of blood. Thank you to all those who regularly donate these blood products. Dad is a large consumer!
Day +15, Sunday, April 17th.
WBC: 0.13 k/uL CRITICAL H: 8.7 g/dL LOW P: 79 k/uL LOW Cr: 3.4 HIGH Na+: 147 HIGH
Blood. Dad’s white blood cell count continued to rise. His central line catheter continued to test positive for the atypical Gram-negative bacteria, Achromobacter xylosoxidans. Continued minocycline.
Dad continued to receive blood support (platelet and blood transfusions & neupogen shots) as needed.
Graft versus host disease (GvHD). Sirolimus was restarted since the feeding tube was inserted.
Mouth & Throat. Dad continued to have pain from mucositis and used magic mouthwash to treat.
Heart. Dad blood pressure improved and remained stable.
Lungs. Dad continued to receive supplemental oxygen. Continued voriconazole and acycolovir.
Abdomen. Dad continued meropenem, an ultra-broad spectrum antibiotic. The prior day’s CT scan showed evidence of ileus, which is the inability of the intestine to contract normally and move waste out of Dad’s body.
Kidneys. Dad no longer had blood in his urine. He remained on continuous dialysis. The prior day’s CT scan also showed hydronephrosis, excess fluid in the kidney due to a backup of urine, and hydroureter, dilated ureter. Urology was consulted.
Day +16, Monday, April 18th.
WBC: 0.24 k/uL CRITICAL H: 8.9 g/dL LOW P: 41 k/uL LOW Cr: 1.9 HIGH Na+: 143 NORMAL

Doughnuts from the Mini Doughnut Factory for the ICU staff.
Blood. Dad’s white blood cell count continued to rise. Dad continued to receive blood support (platelet and blood transfusions & neupogen shots) as needed. Weekly testing of CMV and EBV showed positive with decreasing levels. Thus, no treatment prescribed, but will continue to monitor. Dad continued to receive minocycline.
Graft versus host disease (GvHD). Dad continued to receive sirolimus via feeding tube. Acute GvHD assessment resulted in an overall grade of 0.
- Skin = Stage 0
- Liver = Stage 0
- Gut = Stage 0
Mouth & Throat. Dad continued to have pain from mucositis, grade 1, and used magic mouthwash to treat.
Heart. Dad was in and out of atrial fibrillation. Continued metoprolol to address. Blood pressure continued its improvement.
Lungs. Continued voriconazole and acycolovir. Dad continued to receive supplemental oxygen, but lowered oxygen flow from 10L to 6L. Continued to have productive coughs. Kept Dad more upright in bed (no less than 30 degrees).
Abdomen. Began tube feeds to provide Dad nutrition. X-ray taken.
Kidneys. Dad remained on continuous dialysis. Doctor considered moving Dad from continuous dialysis to 4 hour dialysis.
Day +17, Tuesday, April 19th.
WBC: 0.55 k/uL CRITICAL H: 9.2 g/dL LOW P: 40 k/uL LOW Cr: 2.3 HIGH Na+: 145 NORMAL
Blood. Dad had his central line catheter removed. It was an extremely painful event. The surgical scissors/tweezer tip broke off and remained in Dad’s chest near his right, third rib. The broken piece was subsequently retrieved. Later another painful event for Dad was that the PICC team was unsuccessful in placing a PICC line in Dad’s arm.
He continued to receive minocycline.
Dad’s white blood cell count continued to rise. Dad continued to receive blood support (platelet and blood transfusions & neupogen shots) as needed.
Graft versus host disease (GvHD). Dad continued to receive sirolimus via feeding tube. Acute GvHD assessment resulted in an overall grade of 0.
- Skin = Stage 0
- Liver = Stage 0
- Gut = Stage 0
Mouth & Throat. Dad continued to have pain from mucositis, grade 1, and used magic mouthwash to treat.
Heart. Dad was in and out of atrial fibrillation. Continued metoprolol to address. Cardiology was following.
Lungs. Dad continued to receive supplemental oxygen, but lowered oxygen flow from 6L to 2L. Continued to have productive coughs. Continued voriconazole and acycolovir.
Abdomen. Continued tube feeds.
Kidneys. Dad had no dialysis. Considered moving Dad back to BMT (Blood & Marrow Transplant) unit from ICU.
Mentation: Dad was disoriented to place and time.
by Jena | Apr 17, 2016 | Atrial Fibrillation, BK virus, Dialysis, Graft-versus-host-disease (GvHD), Infectious Disease, Meropenem, Minocycline, MRSA, Sepsis, Sirolimus, Stem Cell Transplant, Zosyn |
 Dad was moved to the ICU on the second floor.
Dad was moved to the ICU on the second floor.
Day +13, Friday, April 15th.
WBC: 0.08 k/uL CRITICAL H: 7.4 g/dL LOW P: 18 k/uL LOW Cr: 3.9 HIGH Na+: 148 HIGH
Blood. All three lines (blue, red & white) in Dad’s central line catheter indicated Gram-negative bacteria. Continued minocycline for MRSA and atypical Gram-negative bacteria.
Dad continued to receive blood support (platelet and blood transfusions & neupogen shots) as needed.
Graft versus host disease (GvHD). Dad was unable to take sirolimus since he was restricted from all food and drink.
Mouth & Throat. Dad continued to have pain from mucositis and used magic mouthwash to treat.
Heart. The day before’s echo cardiogram confirmed no heart failure.
Lungs. Dad continued his liquid diet. Again, anytime he drank, he would go into a terrible coughing fit and would require use of an oral suction/vacuum. It was determined that Dad’s epiglottis was not closing properly to prevent food and drink from entering his larynx down to his lungs. The day before’s two chest X-rays showed developing aspiration pneumonia.
Dad had another X-ray taken of his chest. Continued supplemental oxygen. Ordered a nasal feeding tube, but the nurse, who specializes in feeding tube insertions, was unsuccessful in placing Dad’s tube after several attempts.
Abdomen. The day before’s abdomen X-ray showed mild improvement. Imodium was stopped. Dad was switched from Zosyn to meropenem, an ultra-broad spectrum antibiotic.
Kidneys. Nephrology discussed with us the possibility of Dad needing dialysis. The day before’s renal ultrasound showed swelling of Dad’s right kidney due to a possible obstruction. Repeated ultrasound. BK virus was finally confirmed as the source of blood in Dad’s urine. Continued IV fluids and monitored sodium levels. Nephrology also monitored potassium in Dad’s blood and identified Dad as having hypokalemia (deficiency of potassium in the bloodstream). Dad was considered anuric (not passing urine).
Legs. An ultrasound of Dad’s legs, taken the night before, confirmed no blood clots.

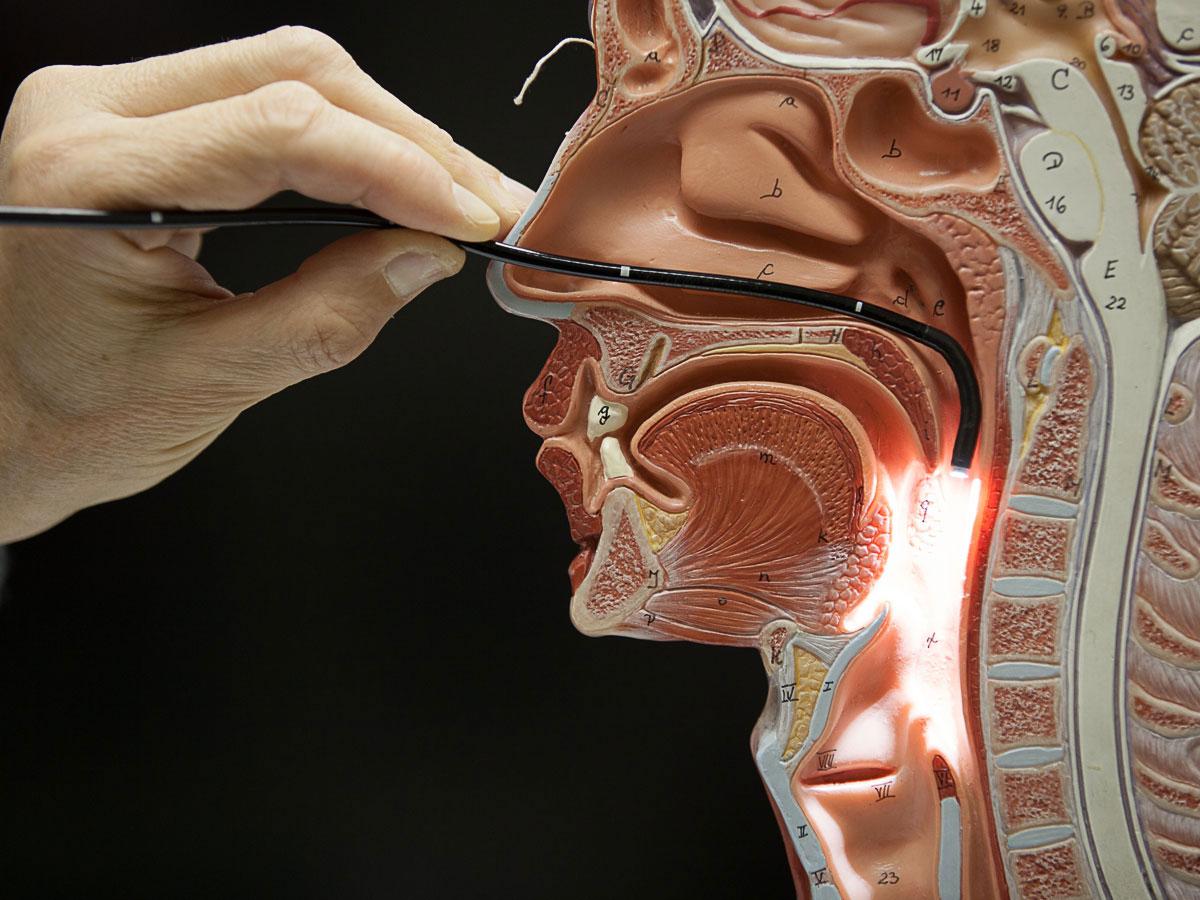 Mouth and Throat. Based upon the result of the CT scan of Dad’s brain, ENT (ear, nose & throat) was consulted to check for fungal sinusitis. ENT performed a bedside Flexible Nasal Endoscopy, which showed no evidence of a fungal infection. It did show a clear, runny nose. ENT recommended continued IV antibiotics for viral and bacterial sinusitis.
Mouth and Throat. Based upon the result of the CT scan of Dad’s brain, ENT (ear, nose & throat) was consulted to check for fungal sinusitis. ENT performed a bedside Flexible Nasal Endoscopy, which showed no evidence of a fungal infection. It did show a clear, runny nose. ENT recommended continued IV antibiotics for viral and bacterial sinusitis.
 Dad was moved to the ICU on the second floor.
Dad was moved to the ICU on the second floor.
Recent Comments