by Jena | Dec 30, 2015 | Stem Cell Transplant |
 This morning we attended the Allogeneic Pre-Transplant Class at Moffitt. It was our first time in the transplant inpatient unit as the class was held in 4W (fourth floor of the Moffitt inpatient area, west wing). Transplant inpatients are located on the third and fourth floors providing 18 private rooms per floor. Transplant patients, who require additional hospitalization due to post-transplant issues, use these same rooms unless the issues are life-threatening and the patient requires ICU.
This morning we attended the Allogeneic Pre-Transplant Class at Moffitt. It was our first time in the transplant inpatient unit as the class was held in 4W (fourth floor of the Moffitt inpatient area, west wing). Transplant inpatients are located on the third and fourth floors providing 18 private rooms per floor. Transplant patients, who require additional hospitalization due to post-transplant issues, use these same rooms unless the issues are life-threatening and the patient requires ICU.
Today’s class started with a diet technician. She provided nutrition guidelines for transplant patients. She mostly covered the details of the immunosuppressed diet. Dad will remain on the immunosuppressed diet from as short as a few months to much longer…over a year. Dad has always been fairly germaphobic. This trait may serve him well post-transplant and reduce his risk of infection.
After the transplant, Dad’s neutrophil count must be >500 to be discharged.
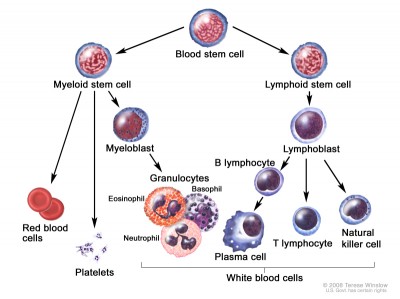
Next, Michele Stratton, RN, BMTCN, went over many aspects of the pre-transplant process. She started with the basics of what a stem cell is. A key measure to watch, after the transplant has occurred, is the neutrophil count. The count must be 500 before Dad will be discharged. He will have blood drawn everyday between 3:00am and 5:00am each morning.
I appreciated learning about the donor stem cell collection process. What a blessing stem cell donors are! They are truly saving lives. If you are between 18 and 44, give consideration to becoming a donor.
Yesterday, I mentioned in my post about the conditioning chemotherapy given just prior to the transplant. Michele spoke about the side effects of some of the chemotherapy drugs. The worst of the conditioning therapy side effects usually occur at Day +8, Day +9, and Day +10. They include the typical list of nausea and vomiting, diarrhea, decreased appetite, mucositis, hair loss, fatigue, changes in memory and concentration, decreased blood cell counts, and infection.

55 MS Powerpoint slides from today’s class.
Melphalan is one of the two chemotherapy drugs Dad is to receive. Unfortunately for Dad, Melphalan is one drug that produces mucositis (mouth sores). Dad experienced severe mucositis when he was being treated with Folotyn this summer. He was in terrible pain and unable to eat. Dad was so miserable he required prescription pain medication. I remember bringing him lots of milkshakes, which he could drink with a straw. The straw helped bypass the sores in his mouth. Michele stated that cryotherapy right before, during, and after the Melphalan infusion could help reduce the mucositis side effect. The cryotherapy is simple in concept but harder to execute. Dad will need to hold ice chips in his mouth for about 45 minutes. This does not mean simply chewing on some ice chips, but rather holding the chips on his tongue, continuously, for the 45 minutes. The ice will cause the blood vessels in his mouth to constrict and reduce the amount of Melphalan impacting his mouth.
On Day 0, when the stem cells are infused, Dad may receive pre-medications to prevent reactions to the donor’s stem cells. Pre-medications are driven by how much of a match the donor is and blood type, The closer the match the less pre-medications. We need to find out how close of a match Dad’s donor is.
Dad is not looking forward to being in the hospital for 3 to 3.5 weeks. Michele suggested items Dad should consider having in his room while he is an inpatient. She discouraged long, complex novels since most patients experience a change in concentration as a chemotherapy side effect. Additional items we are considering:
- Bose or Beats wireless speaker (Dad can play music from his iPhone)
- Apple TV (Dad can binge watch shows)
- Skull cap/beanie (Grandson can pick Dad out a few nice Nike and Under Armour skull caps)
Graft-versus-host-disease (GvHD) was discussed at length. Dad’s doctors are counting on some amount of graft-versus-tumor to eliminate any residual cancer. Thus, a little bit of GvHD is beneficial, but mostly it is not. Acute GvHD occurs within the first 100 days after the transplant. Chronic GvHD generally occurs within the first two years after the transplant.
Dad doesn’t have any Moffitt appointments for the remainder of the week. He deserves this short break before he starts radiation on Monday.
by Jena | Dec 29, 2015 | Stem Cell Transplant |

The pre-transplant train continues to move along its tracks. We met with Denise, the transplant coordinator, this morning. She shared that Dad has a tentative transplant admission date of February 4th and a transplant date of February 9th. Denise is awaiting confirmation from the two donors that one of them is available to donate according to this new proposed date. Denise reviewed the four consents that we will need to sign when we meet with Dr. Ayala, Dad’s transplant doctor, on January 8th.
One of the consents is for the two chemotherapy drugs to be administered starting Day -5 when Dad is admitted on February 4th. The two drugs are Fludarabine and Melphalan and seem to be the standard Moffitt transplant conditioning regimen. Last night, I ran across a recent article, “The rarest of rashes,” in the Stanford Medicine magazine, which describes how Stanford is now skipping the chemotherapy that has been considered a prerequisite to stem cell transplant for CTCL patients. Instead, the Stanford team is preparing each patient for transplant in a customized way by tailoring a combination of drugs and radiation that the Stanford team believes is most applicable to the patient’s disease. The goal of the customized approach is to reduce the spread of the disease as much as possible and eliminate skin tumors before transfusing the donor’s stem cells to eliminate any remaining disease in the patient. I inquired about the new Stanford method with both Denise, the transplant coordinator, and Karla, the transplant PA. Neither seemed to be familiar with this new Stanford method, but they did encourage me to ask Dr. Ayala when we meet with him next week.
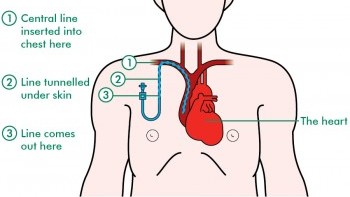
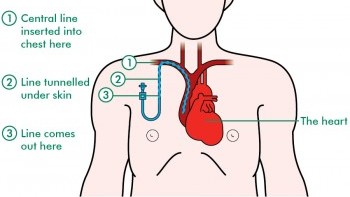
Central catheter line. Image from http://www.macmillan.org.uk/
On February 3rd, Dad will have his PICC (peripherally inserted central catheter) line removed and a central catheter line inserted. He will be sedated. A minimum platelet count of 50 (50,000) is required for the procedure. Denise, the transplant coordinator, believes that Dad may need a platelet transfusion prior to the procedure since his platelet count continues to be low. The central catheter line will remain until approximately 4- 6 weeks post transplant. The timing will be driven by Dad’s blood counts and ability to clot (platelets). At that time, the central catheter line will be removed, and a port will be inserted.
Denise indicated that there was no firm decision about brentuximab vedotin from the doctors. Karla believed that it may be used during post transplant. Thus, Dad sent an email to Dr. Sokol, malignant hematology, and Dr. Ayala, transplant, inquiring about using brentuximab vedotin as a systemic treatment.
One of the last topics discussed with Denise was graft versus host disease (GvHD). It is a condition that might occur after the transplant. Dad may experience acute GvHD and/or chronic GvHD. Denise described the symptoms of GvHD. One of the symptoms is a rash, which is also how CTCL appears. A skin punch biopsy would be done to determine if it is GvHD or the return of CTCL.
In the BMT Treatment Center, Dad received a blood transfusion today since his hemoglobin level had dropped from yesterday from 7.7 to 7.1. Only one unit today since Dad’s schedule was full with other appointments including more vital organ function testing (EKG and ECHO). Karla went ahead and scheduled Dad for a second unit tomorrow.
by Jena | Dec 28, 2015 | Stem Cell Transplant |

BMT Clinic at Moffitt Cancer Center.
Today was Dad’s first day of five pre-transplant testing days. The day started in the BMT (bone marrow transplant) clinic with a visit with Theresa, the social worker who was filling in for Penny, who is out of the office this week. Penny is the social worker assigned to Dad. The social worker is a member of the transplant team responsible for providing assistance with resources such as local housing and for providing family or individual support and counseling. Theresa asked Dad a number of questions to obtain a view of his physical and mental history. Mom and I responded to caregiver questions since we are serving as the primary and secondary caregivers, respectively.
Moffitt Cancer Center Allogeneic Transplantation Patient and Caregiver Guide.
A main topic of discussion and of high importance to Mom and Dad was nearby lodging required for the first 75 days after being discharged from Moffit post-transplant. The rule of thumb is that the Dad would need to be within 30 minutes of Moffitt. Dr. Ayala, Dad’s transplant doctor, and Denise, the transplant coordinator, made it clear during our initial BMT visit this summer that Dad would have to reside closer to Moffitt than their condo in South Tampa. On a good day without traffic, the drive to Moffitt from South Tampa would take no more than 20 minutes. Unfortunately, traffic and South Tampa flooding are unpredictable. Anyone living in South Tampa this summer experienced heavy flooding multiples times, which resulted in many impassable roads. Mom was disappointed to hear that the Hope Lodge is closed for renovations and is scheduled to reopen in April. The Hope Lodge is conveniently located across the street from Moffitt. Our lodging options are now Marriott’s TownePlace Suites, Marriott’s Residence Inn, and the Lodges at Lake Crest. All are located approximately ten minutes from Moffitt. Both Marriott hotels provide shuttle service to and from Moffitt. Mom stressed the need for excellent cleaning services. We learned that Moffitt procures its own cleaning services for the Moffitt rooms at the hotels since the transplant patients are at high risk of infection.
This afternoon, Denise, the transplant coordinator, provided the results of Dad’s bone marrow biopsy and skin biopsy. The bone marrow biopsy showed some chromosomes that may be an early indicator of Myelodysplastic syndrome (MDS). The good news is that Dad’s bone marrow seems to be ever-so-slowly recovering from the pancytopenia caused by his Campath treatments. This morning Dad had a blood draw to check his counts and to determine if he needed a blood transfusion today. Dad’s platelets are up to 32 (32,000) from 19 (19,000) a couple weeks ago. (A normal platelet count ranges from 150,000 to 450,000 platelets per microliter of blood.) His hemoglobin was 7.7. (For men, a normal hemoglobin level ranges from 13.5 to 17.5 grams per deciliter). Dad did not need a blood transfusion since his hemoglobin was >7.0.
The skin biopsy indicated the presence of CD30. This is actually good news in that Dr. Sokol, malignant hematology, may be able to treat Dad systemically with brentuximab vedotin, which is an anti-CD30 monoclonal antibody and is less toxic than chemotherapy. Dad’s bone marrow, immune system and blood are unable to withstand any chemotherapy treatments at this time. Our hope is that a systemic treatment will address Dad’s internal tumors.
Dr. Ayala, transplant doctor, wants to execute the transplant as soon as Dad completes his radiation treatment. Thus, we are assuming an early February transplant. Since both of Dad’s siblings passed earlier in life, Dad had to find a match through the donor database. Dad is blessed in that he has two matches. Both donors are located outside of the United States. Truly amazing.
by Jena | Dec 23, 2015 | Radiation Therapy, Stem Cell Transplant |
Yesterday, Dad met with Dr. Montejo, radiology oncology, to discuss and plan for his radiation treatment. As a part of that discussion, Dr. Montejo shared Dad’s latest PET (positron emission tomography) scan, which was taken November 24, 2015. Dr. Montejo stated that numerous “spots” have appeared in Dad’s scan. They are not only on/in Dad’s skin, but tumors have appeared in a lymph node (groin – right side) and his bones. The two most significant spots in his bones are his lower spine and his rib cage on the right. Dr. Montejo wanted to know if Dad had been experiencing any issues with his lower back, but Dad has not noticed any pain there. No cancer was seen in his organs.
We are extremely saddened by the news of these tumors, but grateful of the time and attention that Dr. Montejo gave to Dad in sharing the PET scan results and discussing ways to treat the tumors. Dr. Montejo spoke with Dr. Sokol, malignant hematology, and Dr. Ayala, bone marrow transplant (BMT), and communicated the radiation treatment plan to them. We are awaiting word from Dr. Ayala and Denise LaFave, transplant coordinator, about the current stem cell transplant schedule of activities, which are supposed to begin next week. We do not know if the transplant activities will be delayed or put on hold due to these new tumors.

Henry B. Plant Museum’s Victorian Christmas Stroll
Today, Dad went in for his radiation simulation. The simulation was done in preparation for the radiation treatment. Detailed imaging scans were done to show the exact location of Dad’s tumors. Treatment begins January 4th and runs throughout January. The phases of the current radiation plan are:
- Treat the internal tumors
- Treat the subcutaneous tumors (leg & arm)
- Treat the cutaneous tumors
Mom works incredibly hard, 24 hours a day, providing Dad the BEST care anyone can receive. She deserves more breaks than she gets the opportunity to take. This morning we took Mom to the Henry B. Plant Museum’s Victorian Christmas Stroll. She was able to experience a bit of that Christmas spirit we all need right now.
 This morning we attended the Allogeneic Pre-Transplant Class at Moffitt. It was our first time in the transplant inpatient unit as the class was held in 4W (fourth floor of the Moffitt inpatient area, west wing). Transplant inpatients are located on the third and fourth floors providing 18 private rooms per floor. Transplant patients, who require additional hospitalization due to post-transplant issues, use these same rooms unless the issues are life-threatening and the patient requires ICU.
This morning we attended the Allogeneic Pre-Transplant Class at Moffitt. It was our first time in the transplant inpatient unit as the class was held in 4W (fourth floor of the Moffitt inpatient area, west wing). Transplant inpatients are located on the third and fourth floors providing 18 private rooms per floor. Transplant patients, who require additional hospitalization due to post-transplant issues, use these same rooms unless the issues are life-threatening and the patient requires ICU.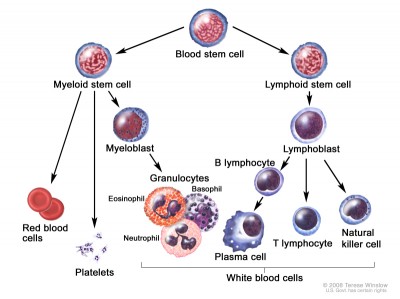





Recent Comments