by Jena | Mar 31, 2016 | Fludarabine, Infectious Disease, Melphalan, Stem Cell Transplant |
Day -5, Sunday, March 27: Dad got settled into his room in the BMT (blood and marrow transplant) unit on the third floor of the Moffitt Cancer Center. His room is just a few doors down from his prior room in early March. Dad met with Dr. Ochoa, inservice BMT doctor, and Karla Adams, inservice BMT physician assistant. Dr. Ochoa is a jokester, which means that Dad will enjoy his visits with Dr. Ochoa. Karla was extremely friendly, as usual, providing Mom and Dad with hugs.
Mid-afternoon, Dad viewed our church’s Easter service online. Afterwards, Dad received some fluids intravenously (saline).
Dad was slightly pleased with his Moffitt dinner and claimed that it was better than before. After Dad finished dinner, he and Mom walked a mile (11 laps in the BMT unit).
Around 9:00 p.m., Dad started receiving pre-meds for his fludarabine (1st of 4), the conditioning chemotherapy. The earlier plan was for Dad to take steroids as a pre-med for each conditioning chemotherapy. However, Dr. Ochoa gave Dad a milder anti-nausea and anti-vomiting pre-med instead. Dad got along fine with these changes. The purpose of the conditioning therapy before a stem cell transplant is to destroy the cancer cells in the body. The dosage received is much higher during conditioning therapy than in the course of normal treatment. Dad didn’t experience any negative side effects during the infusion.
As anticipated, Dad has already met some of his neighbors, Dan and Jamie. Both are younger. Mom and Dad guessed that they are in their 30s. Dan and Jamie are a few days ahead of Dad in the stem cell transplant process.
 Day -4, Monday, March 28: This was Dad’s real birthday. He turned 76!
Day -4, Monday, March 28: This was Dad’s real birthday. He turned 76!
Dad had a good night’s rest. Mom tried out the pull out sofa in Dad’s room last night. She found it to be rather hard. Dad had breakfast and walked one mile in the morning. Dad then saw Dr. Ochoa, who was very pleased with Dad’s status and talking.
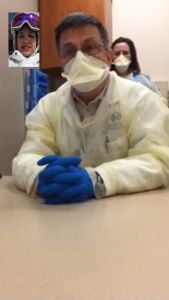
Dad saw Dr. Baluch, BMT infectious disease, in the afternoon. She changed one of Dad’s medications and cautioned him as he is very suspectible to infection. His CD4 count was 30. The normal count is 500. Dr. Baluch said that Dad has to be very careful and follow their instructions to minimize the risk of infection.
In the evening, Dad’s pre-meds got started around 9:30 p.m. His fludarabine (2nd of 4) started flowing about 10:00 p.m. He didn’t experience any negative side effects.
Day -3, Tuesday, March 29: Dad had breakfast and then walked a mile. He saw Dr. Ochoa, inservice BMT. Dad’s Moffitt provided lunch was chef salad, pasta with chicken, and carrot cake. Dad spent some time on his laptop. Later in the day, Dad walked two more times at half a mile each. His goal is to walk two miles everyday.
Husband picked Mom up from Moffitt after Dad’s evening shower so that she could do some laundry and get a solid night’s rest at home.
Since we came home from spring break, I haven’t been able to visit Dad, in person, due to my being ill. Each day, Mom and Dad ask if I am feeling better. They are eager to have me visit in person rather than via FaceTime.
Dad received his fludarabine (3rd of 4) later in the evening with no negative effects.
Day -2, Wednesday, March 30: Dad woke up feeling fine. Husband picked up Mom at 9:00 a.m. and took her to the Moffitt Cancer Center. Sweet Daughter had offered to lend Dad her Bose wireless speaker so that Dad could listen to music on his iPhone. Husband visited with Dad and setup the speaker with Dad’s iPhone.
Dr. Ayala, Dad’s BMT doctor, stopped in to visit Dad. This made Mom and Dad very happy.
Mom went to the optional caregivers gathering, which occurs each Wednesday. Mom found it to be interesting and very informative. She learned that each BMT patient, currently in the BMT unit, has a different form of cancer.
This was the last day of Dad’s conditioning  chemotherapies…the double-doozie of fludarabine (4th of 4) and melphalan. Melphalan is the chemotherapy that is likely to give Dad mouth sores, oral mucositis. These usually appear 5 – 10 days after the melphalan is received. Mucositis can then last 7 – 14 days. To minimize Dad’s risk of getting mucositis, Dad used oral cryotherapy. The idea behind the oral cryotherapy is to make the mouth cold enough that the blood vessels in the mouth constrict and reduce the amount of Mephalan in the mouth. Dad packed ice pellets into every nook and cranny of his mouth and contained them in his mouth for 75 minutes. He went through four cupfuls of ice. Dad found it to be quite the challenge. Mom claimed that Dad was screaming while his mouth was full of ice.
chemotherapies…the double-doozie of fludarabine (4th of 4) and melphalan. Melphalan is the chemotherapy that is likely to give Dad mouth sores, oral mucositis. These usually appear 5 – 10 days after the melphalan is received. Mucositis can then last 7 – 14 days. To minimize Dad’s risk of getting mucositis, Dad used oral cryotherapy. The idea behind the oral cryotherapy is to make the mouth cold enough that the blood vessels in the mouth constrict and reduce the amount of Mephalan in the mouth. Dad packed ice pellets into every nook and cranny of his mouth and contained them in his mouth for 75 minutes. He went through four cupfuls of ice. Dad found it to be quite the challenge. Mom claimed that Dad was screaming while his mouth was full of ice.
 Day -1, Thursday, March 31: Dad started his “off day” with a large breakfast of french toast, sausage and donuts. It was an off day in that Dad had a day of rest. No more conditioning chemotherapies. Dad was feeling good and enjoying a new album I gave him for his birthday, Gone Like the Cotton from the Cox Family, which was produced by Alison Krausse. Dad’s favorite song on the album is “Cash on the Barrelhead.”
Day -1, Thursday, March 31: Dad started his “off day” with a large breakfast of french toast, sausage and donuts. It was an off day in that Dad had a day of rest. No more conditioning chemotherapies. Dad was feeling good and enjoying a new album I gave him for his birthday, Gone Like the Cotton from the Cox Family, which was produced by Alison Krausse. Dad’s favorite song on the album is “Cash on the Barrelhead.”
Dad walked his two miles in three phases. Later in the evening, after Dad’s bedtime shower, Husband picked up Mom so that she could get quality sleep in her own bed.
While sitting in his lounger that night, Dad experienced some tremors in both hands and arms.
by Jena | Mar 27, 2016 | Fludarabine, Stem Cell Transplant |
Early in the week, we were notified that Dad’s transplant admission date was moved from Thursday, March 24th to today, Sunday, March 27th per the donor’s request. I have learned that the plan is that it never goes as planned. This delayed admission date, along with Dad’s strong insistence, encouraged me to fly out West on Tuesday to spend spring break with Husband, Son, and Daughter.
How apropos that Dad’s new admission date is Easter Sunday, and our church’s Easter sermon is “New Life Starts Here!”

FaceTiming with Dr. Ayala and Diane
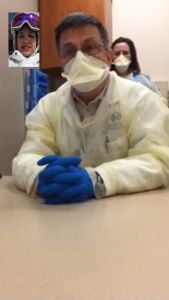
On Thursday while on the mountain, I virtually participated in Dad’s pre-admission appointment with Dr. Ayala, transplant doctor, via FaceTime. I felt comfortable participating virtually since Dad has had two of these appointments in the past prior to his previous admission delays. The appointment was rather routine in that Dad’s medications were reviewed. Dr. Ayala conducted a physical exam. Dr. Ayala confirmed that we were well aware of the risks and acknowledged that we have had this “risk” discussion several times now. Diane, transplant coordinator filling in for Denise, provided an updated calendar depicting day-by-day transplant activities.

Kubi by Revolve Robotics
Dad continues to be amazed by today’s technologies. Husband and I have been discussing additional technologies that would allow us to be in Dad’s room, during his monthlong stay, when we cannot be there the moment the team of doctors make rounds each day. A high-end solution, Double 2 by Double Robotics, is being used in hospitals today. One example is of a teenage lymphoma patient continuing to attend school virtually from his hospital room. I personally like the Kubi by Revolve Robtics as a moderately priced solution.
Dad called the Moffitt Cancer Center this morning to confirm a noon availability of his bed on the BMT (blood & marrow transplant) floor…his bed is ready and waiting for him. If it had not been ready, he would have gone to the BMT clinic at noon to get his first conditioning chemotherapy, Fludarabine, underway while waiting for his bed to become available. During Dad’s Thursday appointment, Diane shared that there are currently 7 or 8 inpatients in progress with their stem cell transplants. Dad will be moving into their BMT neighborhood. Knowing Dad, he will chat them all up within the first few days of admission. I hope they are ready for Chatty Daddy.
Dad’s journey to a new life begins today. Alleluia!
https://youtube.com/watch?v=PBvU7arNhQs%3Frel%3D0
by Jena | Mar 17, 2016 | Stem Cell Transplant |
Mom and Dad called me yesterday to notify me that Dad’s new admission date for his stem cell transplant is Thursday, March 24th, which is exactly one week from today.
During this week, our family will be traveling to various parts of the country. Daughter and Son’s school spring break starts tomorrow. Daughter is off to space camp tomorrow, and Son is off to Savannah on Saturday. After they return back to Tampa, the family is scheduled to fly out west to go skiing.
I am “battling” Mom and Dad about staying in Tampa to be with them. Of course, selfless Dad is doing his best to force me go skiing with the family. I know he feels terrible and full of guilt at the thought that I would be missing the opportunity to spend family time with Husband, Son and Daughter. Dad even took that authoritative “I’m your father” tone of voice with me yesterday. Mom and Dad were trying to convince me that the doctors and nurses would be doing all the work and that there would be nothing for me to do. I understand that I cannot take medical action, but I have learned how important it is to have 3 sets of ears versus two when meeting with the medical team. Mom and Dad countered with the promise to call me when the medical team visits Dad. I argued that Dad is the most important person in the family at this point in time, and he needs to come first.
We shall see. We will be out west before Dad goes into the hospital. I am contemplating returning home early. To add more guilt to the mix, Husband suggested that he, Son and Daughter fly home with me. And, Daughter said she only wants to ski with me. I know that is not really a true statement. Thus, if I don’t go, she doesn’t want to go. Then, we have Son who has been counting down the days to snowboarding since Christmas. Ugh. I am adamantly against the idea of anyone returning to Tampa with me or staying home with me.
The planner in me wants to make a plan. We have learned that Dad’s schedule seems to invariably shift. I have to get out of my comfort zone and take it day by day.
Now, I am hearing in my head the song, by the Clash, “Should I stay or should I go?”
https://youtube.com/watch?v=oGIFublvDes%3Frel%3D0
by Jena | Mar 14, 2016 | Brentuximab Vedotin, Infectious Disease, Stem Cell Transplant |
Monday, March 14th at 2:00 p.m., Dad had his follow-up appointment with Dr. Ayala at the main campus of the Moffitt Cancer Center. The appointment started with Denise, transplant nurse, reviewing Dad’s current medications. She also asked about Dad’s current symptoms. Denise noted that Dad’s last blood transfusion was two days ago on Saturday.
Dad immediately asked Denise if she had a new transplant admission date. She did not. Denise said that Dr. Ayala had not allowed her to schedule the donor until he saw Dad. Denise anticipated Dr. Ayala would now allow her set a new admission date with the donor based upon what she was seeing and hearing during the appointment. She sought to manage Mom and Dad’s expectations by saying that the admission date would likely be at least seven days out. Dad expressed disappointment with the week long wait. According to Denise, it is common courtesy to provide the donor time to make plans to accommodate the transplant date. Denise also shared that Dr. Ayala had reached out to Dr. Sokol, hematology oncology, asking if Dad needs another dose of Brentuximab Vedotin.
At 2:45 p.m., Dr. Ayala came in and asked how Dad was feeling. Dad’s biggest complaint was in regards to his feet and legs due to their over radiation. They burn, tingle and randomly go numb. Dr. Ayala inquired of his appetite and his fitness. Dad has been going to the fitness center, exercising in a mask and gloves, every few days. Dad spends 20 minutes on the bike and does some free weights. I imagine that Dad has no problem getting on a bike nor accessing the weights. Others, in the fitness center, probably scurry away thinking Dad has some highly infectious disease when they see him wearing his mask and gloves. A perk of being immunosuppressed.
Dr. Ayala conducted a physical examination of Dad. The egg, which now looks like a black mushroom, on Dad’s head is starting to reduce in size. Dad calls it a “head decoration.” Dr. Ayala said that Dad’s skin looked perfect. Dr. Ayala checked Dad’s lungs, legs and feet. At the end of the physical exam, Dr. Ayala asked jokingly, “What are we going to do with you?”
Dr. Ayala observed that Dad has gotten weaker. Dr. Ayala said that he doesn’t have a solid reason not to proceed with the stem cell transplant. He stated that without a transplant, Dad has no chance for survival. Dr. Ayala increased the risk of Dad dying from the transplant to 30-40%. Dr. Ayala predicted that it will be a bumpy road, and it may not work.
Dad wanted to know about the status of his disease. Dr. Ayala said that Dad still has CTCL. It is well under control, but no for a long time. It will come back and in full force. From a CTCL point of view, Dad looked “beautiful.” Disease control was excellent. His blood and skin had cleared.
Mom inquired about Dad’s weight loss. We reviewed the trends displayed in Dad’s weight graph on the exam room computer. Since January, Dad has lost 14 pounds. Dr. Ayala instructed Dad to continue going to the gym, walk, get stronger, be cautious about infections, eat, and fatten up.
Dr. Ayala recommended that Dad not do another round of Brentuximab Vedotin since they are targeting an admission date of a week or less.
 Denise will work with Mark, PA at Moffitt Cancer Center at International Plaza (MIP), to setup appointments for regular blood support and a daily line flush until
Denise will work with Mark, PA at Moffitt Cancer Center at International Plaza (MIP), to setup appointments for regular blood support and a daily line flush until
Dad’s new admission date for transplant.
Dr. Ayala and Denise will determine the proper Bactrim dosage (the script says one amount and the medicine bottle says another). Denise will notify Dad about the donor and the confirmed admission date. Denise will develop and send Mom a new, custom calendar containing Dad’s key activities during the transplant.
Hopefully, the fourth time is a charm!
by Jena | Mar 14, 2016 | Infectious Disease, Stem Cell Transplant |
Since Dad’s discharge as an inpatient in the Blood & Marrow Transplant (BMT) unit at the Moffitt Cancer Center on March 1st, Dad has been going daily to Moffitt to have his central line catheter flushed and to receive blood support. He has been given blood transfusions to elevate his hemoglobin (red blood cells), platelet transfusions, and neupogen shots to increase his white blood cell count. During this time, Dad was also taking Bactrim to treat his PJP and voriconazole to address potential fungal nodules in his lungs.
On Wednesday, March 9th, Dad had his follow-up CT scan at the Moffitt Cancer Center at International Plaza (MIP). Late that afternoon, Dad received a phone call from Dr. Ayala’s office stating that Dr. Ayala would not be able to see him as originally planned on Thursday, March 10th. Dr. Ayala had the flu. Dad’s appointment was then rescheduled for Monday, March 14th. Mom and Dad were highly disappointed. They had set their sights on Sunday, March 13th, as an inpatient admission to the BMT unit for Dad’s transplant….even though no one had given indication of a new admission date nor transplant date. Mom and Dad were extremely eager to get this transplant moving. Dad had experienced so many delays. The delays were weighing down his spirit. Mom was struggling with Dad being disheartened.
Early Thursday morning on March 10th, we went to Moffitt Cancer Center’s main campus to meet with Dr. Baluch, BMT infectious disease. We had actually never met Dr. Baluch when Dad was an inpatient earlier this month. Dr. Baluch had been out ill and then had gone on a ski vacation. We were eager to finally meet Dr. Baluch as her positive reputation had preceded her.
In the Blood & Marrow Transplant (BMT) clinic, we first met with Dr. Baluch’s nurse. She came in to review Dad’s information and medications. The nurse wanted to know about Dad’s respiratory symptoms. Dad said that he always has had a runny now (since he has been getting cancer treatments). Dad did not have a sore throat. The nurse inquired about any fevers, diarrhea, shortness of breath, etc. The nurse took a respiratory virus panel to check the status of Dad’s rhinovirus (aka the common cold).
Dad asked the nurse to assist him in getting in contact with Denise, transplant nurse, or her backup, Diane. Mom seemed to think that Denise was out of the office. Dad needed additional line flush and blood support appointments scheduled through Monday, March 14th, the day of Dad’s appointment with Dr. Ayala.

Dr. Aliyah Baluch
Dr. Baluch, BMT infectious disease, then came in to see Dad. She asked about any history of hemorrhoids, toe nail fungus, and mouth sores. She wanted to know Dad’s travel and career history along with his current living arrangements and hobbies. Dr. Baluch asked how Dad had been feeling the past few days.
We had a long discussion about his “vori” (voriconazole) medication. Dr. Baluch sought to understand when Dad first started taking vori and what dosage. Dr. Baluch confirmed that, from the BAL (bronchoalveolar lavage), two diagnoses were made, rhinovirus and PJP.
Dad successfully finished the two week therapy for PJP. The Bactrim dosage reduction is a precaution to keep Dad from being infected to a new exposure of PJP. Dr. Baluch also wanted to check his vori level via a blood test. It would take about three days to get the results. If needed, she would tweak his vori dosage. She had prescribed vori for Dad as an anti-fungal because he had lived in Ohio during his childhood through college. She indicated that Dad could have picked up something fungal in Ohio earlier during his childhood. The fungus stays with you for life.
Dr. Baluch reviewed the CT scan with us by comparing the prior one from late February to March 9th’s. She was impressed that Dad had cleared so well in only two weeks. It normally takes a minimum of three weeks.
She wanted to check Dad’s CD4 counts by running an immunodeficiency panel considering his numerous atypical infectious disease related infections. It will take one week to get the results back. One way to measure the strength of the immune system of a patient is to measure the T cell count (CD4). CD4 cells are types of white blood cells called T lymphocytes or T cells that fight infection and play an important role in immune system function. This will help her determine risk stratification prior to Dad’s stem cell transplant. Dr. Baluch said that she would be keeping this in her back pocket as a means to make smart decisions about managing Dad’s future risk of infection. Dad will see her when he is an inpatient for transplant.
Dr. Baluch cleared Dad for transplant! She noted that Dad is high risk due to the fact that he has had CMV (cytomegalovirus) and PJP.
Dr. Baluch is extremely engaging and highly impressive. She is Moffitt’s only stem cell transplant infectious disease doctor. She attended medical school, here in Tampa, at the University of South Florida (USF) and did her residency at USF and the Moffitt Cancer Center. Dr. Baluch then moved to the University of Alberta for her fellowship in transplant infectious disease. Subsequently, Moffitt created Dr. Baluch’s current position for her.
After spending time with her on Thursday, I am a firm believer in that every BMT unit must have an infectious disease doctor dedicated to transplant. I say this as no one dies from the actual stem cell transplant itself. Infection remains a major cause of mortality in stem cell transplant patients. Prevention of infection in these patients remains the optimal method of decreasing morbidity and mortality. Once infections occur within a transplant recipient, the mortality rate is high. Pathogens that are benign in an immunocompetent person can lead to significant mortality in transplant recipient patients, who are immunosuppressed.
Our discussion with Dr. Baluch flashed me back to college when I had planned to go to medical school. It reminded me of why I had wanted to be a doctor. I found medicine to be tremendously fascinating and the challenges of saving a life intensely thrilling and purposeful.
I shouldn’t have let my organic chemistry class and the future years of highly expensive medical schooling change my major to engineering.
 Day -4, Monday, March 28: This was Dad’s real birthday. He turned 76!
Day -4, Monday, March 28: This was Dad’s real birthday. He turned 76! chemotherapies…the double-doozie of fludarabine (4th of 4) and melphalan. Melphalan is the chemotherapy that is likely to give Dad mouth sores, oral mucositis. These usually appear 5 – 10 days after the melphalan is received. Mucositis can then last 7 – 14 days. To minimize Dad’s risk of getting mucositis, Dad used oral cryotherapy. The idea behind the oral cryotherapy is to make the mouth cold enough that the blood vessels in the mouth constrict and reduce the amount of Mephalan in the mouth. Dad packed ice pellets into every nook and cranny of his mouth and contained them in his mouth for 75 minutes. He went through four cupfuls of ice. Dad found it to be quite the challenge. Mom claimed that Dad was screaming while his mouth was full of ice.
chemotherapies…the double-doozie of fludarabine (4th of 4) and melphalan. Melphalan is the chemotherapy that is likely to give Dad mouth sores, oral mucositis. These usually appear 5 – 10 days after the melphalan is received. Mucositis can then last 7 – 14 days. To minimize Dad’s risk of getting mucositis, Dad used oral cryotherapy. The idea behind the oral cryotherapy is to make the mouth cold enough that the blood vessels in the mouth constrict and reduce the amount of Mephalan in the mouth. Dad packed ice pellets into every nook and cranny of his mouth and contained them in his mouth for 75 minutes. He went through four cupfuls of ice. Dad found it to be quite the challenge. Mom claimed that Dad was screaming while his mouth was full of ice. Day -1, Thursday, March 31: Dad started his “off day” with a large breakfast of french toast, sausage and donuts. It was an off day in that Dad had a day of rest. No more conditioning chemotherapies. Dad was feeling good and enjoying a new album I gave him for his birthday, Gone Like the Cotton from the Cox Family, which was produced by Alison Krausse. Dad’s favorite song on the album is “Cash on the Barrelhead.”
Day -1, Thursday, March 31: Dad started his “off day” with a large breakfast of french toast, sausage and donuts. It was an off day in that Dad had a day of rest. No more conditioning chemotherapies. Dad was feeling good and enjoying a new album I gave him for his birthday, Gone Like the Cotton from the Cox Family, which was produced by Alison Krausse. Dad’s favorite song on the album is “Cash on the Barrelhead.”


 Denise will work with Mark, PA at Moffitt Cancer Center at International Plaza (MIP), to setup appointments for regular blood support and a daily line flush until
Denise will work with Mark, PA at Moffitt Cancer Center at International Plaza (MIP), to setup appointments for regular blood support and a daily line flush until
Recent Comments